Some Ethical Paradigms In View Of Equipoise and Randomized Clinical Trials
Main Article Content
Abstract
Clinical research on human subjects has been at the epicenter of health care and particularly in ameliorating many diseases. Generally, drugs in Phase III clinical trials are tested on human subjects for "efficacy and potency."[1] Many new invasive therapeutic procedures, too, are tested on human subjects prior to approval. One of the major reasons for clinical research on human subjects is to discover and ascertain a novel way in which a drug, medical device, or therapeutic procedure works in view of treatment of a particular disease or condition. Simply put, clinical trials are sine qua nons in the advancement of medicine and health care. But such trials can become complicated if there are competing treatments for a particular medical situation. In other words, a situation arises when there is a genuine uncertainty in the mind of the researcher or clinical experts of the "...state of genuine uncertainty regarding the comparative therapeutic merits of the interventions being compared in each arm in the trial."[2] This phenomenon is known as equipoise.[3] Equipoise, then, becomes the rational and spring board for randomized clinical trials in order to ascertain the best therapeutic interventions being compared. After all, as the aphorism goes, "it is better to err on the side of caution" than vice versa. Typically, in randomized clinical trials, informed consent may not be obtained, and protocols sometimes are not approved by an institutional ethics review board.
In this piece, I will critically evaluate the threshold for establishing equipoise in view of randomized clinical trials. I will also examine some of the pros and the cons of randomized clinical trials. This paper will explore some ethical challenges especially as they apply to developing countries such as Kenya, Nigeria, and Gabon.
One of the ethical lessons taken from historical precedents, such as the Tuskegee Syphilis study, Nazi medical atrocities, and the subsequent formulation of the Nuremberg Code, is a kind of categorical imperative on researchers to use every known modicum of caution and ethical principle in protecting human subjects during clinical research. The protection of human subjects has become raisons d'être in establishing many ethical guidelines for clinical researchers.
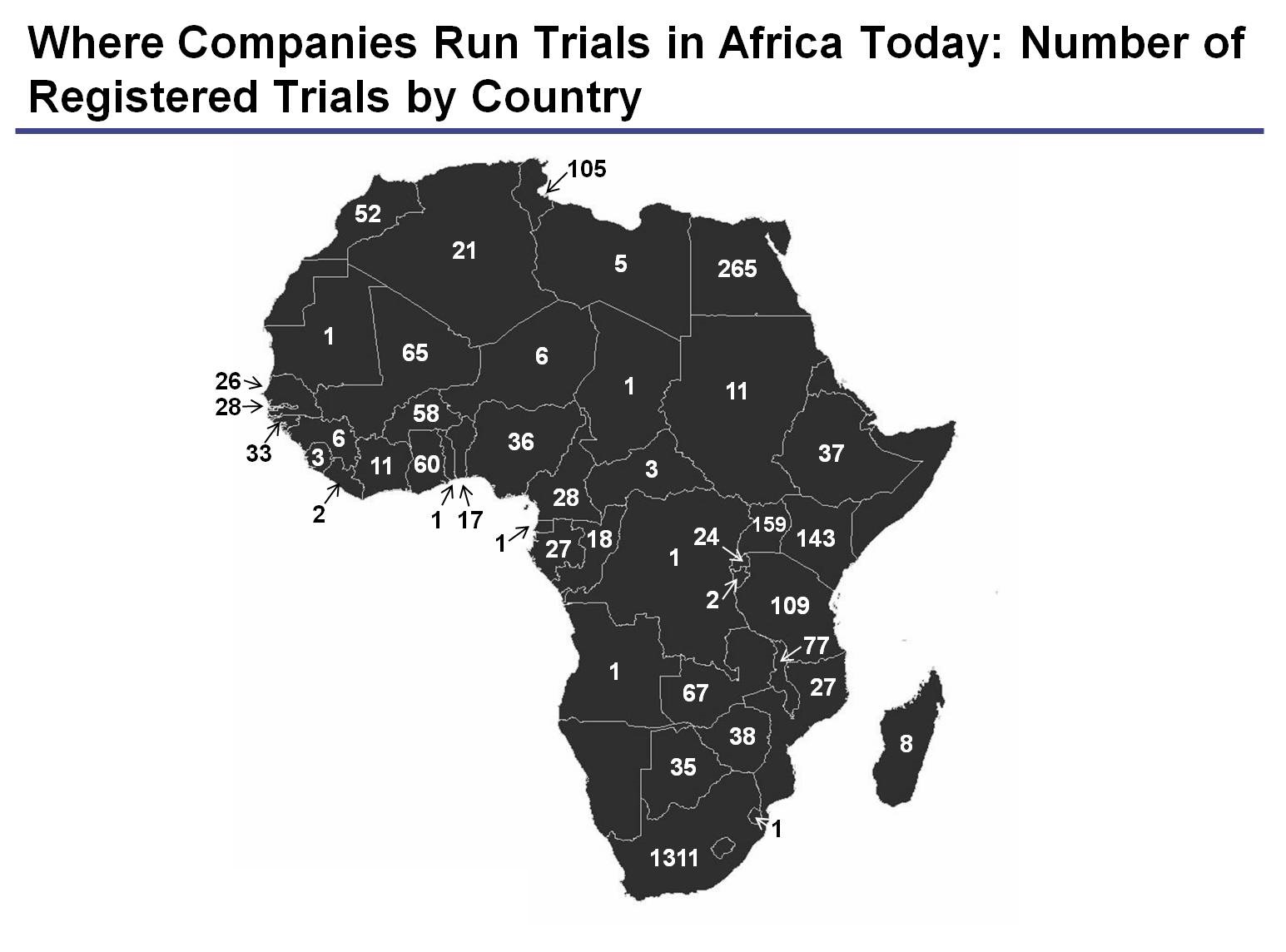
In addition, we have seen a swath of clinical research on the bandwagon in developing and emerging nations. As numerous ethicists are already pointing out, some major challenges are emerging that call for critical analysis and reflection. This becomes even more complicated because human subjects in these countries are particularly vulnerable and resource-limited in terms of access to quality healthcare, dissemination of information, geophysical, socio-economic limitations, as well as subjects' understanding of informed consent and their rights to extricate from any research. These challenges even become egregiously compounded if the research is a randomized clinical trial (RCT) under the aegis of equipoise.
It seems clinical researchers are more meticulous these days and use ethical discretion in order to avoid any danger to human subjects during clinical trials. As a rule of thumb, if a researcher should discover that there are alternative and effective treatments for a specific disease that is the focus of the clinical research; clinical prudence suggests that he ceases his research immediately. However, according to Benjamin Freedman, a phenomenon called clinical equipoisearises when “there is no consensus within the expert clinical community about the comparative merits of alternatives to be tested”. To establish a prima facie case for clinical equipoise, there should be genuine uncertainty in the mind of the researcher or within the medical community, consensus at expert conferences such as AMA, WMA, and within the corpus of medical literature. This is critical in order for any research to begin or continue.[4]
Furthermore, RCT may be construed as ethical if a convincing equipoise is established especially in the context of epidemics or rare diseases. If a clinical equipoise is convincingly established for two competitive drugs/therapeutic procedures for the treatment of the same disease, RCT may be acceptable. In this situation, a plausible inference is that substantial information is known about the efficacy, benefits, and risks of the two competing medications/therapeutic procedures. It is therefore assumed that the study is designed ostensibly to gather more clinical data to improve or enhance medical interventions. This will curtail costs, enhance efficiency, and ensure that human subjects are treated well with either of the medications. For example, a study was carried out comparing Artesunate-Cotrimoxazole and Artesunate-amodiaquine in view of treating asexual and sexual stages of Plasmodium Falciparum malaria in a West African Country where malaria has been consistently prevalent in epidemic proportions.[5] While there are many known medications for treating malaria, it is equally true that the parasite has developed resistance to some drugs such as Chloroquine. Hence, such comparative randomized study using these two drugs in such a clinical trial is novel (at least in my estimation). It also minimizes any serious harm per se because human subjects in both trials were in fact concurrently receiving treatment to a large extent. As these particular treatments concluded, all patients/subjects recovered from malaria within 28 days without any known adverse clinical effects.[6] It is important however to point out that these trials must be fully approved by an IRB or local ethics committee in conformity with international regulatory standards such as the Declarations of Helsinki, if RCT will be used.
It is important to note here that RCT involve a modicum of risk. Furthermore, it is suggested that randomized clinical trials are necessary for the advancement of medicine. These statements are all subtly true. But it becomes serious when human subjects are randomized without any plausible data on the outcomes of the research. However, if the research is non-invasive and involves the use of less toxic drugs during trials, then establishing clinical equipoise as a cogent threshold of minimizing risks in RCT is ethically acceptable; especially, if research subjects are well informed and if these will not influence the integrity of the outcome of the research. I believe these satisfy the ethical requirements for conducting research. For example, a randomized clinical trial was conducted on some adults in Gabon to compare the rate of recovery with Clindamycin in Chloroquine-resistant malaria.[7] The study was on the premise that both drugs cure malaria but there was doubt as to which was better. The study concluded that clindamycin is a good alternative in treating adults with Chloroquine-resistant malaria.[8]
On the contrary, it seems that the flood gates of clinical research trials are opening in emerging and developing countries. It is important to point out also that most of these countries have relatively abysmal health care systems and lack active regulatory bodies with the capacity and resources to monitor clinical trials. The clinical research landscape becomes even complicated as there is an avalanche of local ethos and ethical standards that may be seemingly construed as incongruous to certain international research standards. For example, in certain communities, consent is communitarian. That is, the head of the family, clan, or village may consent on behalf of the subgroup. It becomes complex if RCTs are conducted in these populations that do not guarantee informed consent even if equipoise is established. Should researchers using randomized clinical trials obviate the need for consent? It seems to me that equipoise obfuscates the need for proper consent. This is because equipoise does not warrant clinicians to obtain consent from their patients/subjects during trials. The lack of consent or absence of consent prior to clinical trials violates one of the fundamental requirements of the physician-patient relationship. Informed consent protects both the physician and subjects during research/treatments. We have seen in the annals of medicine how some patients were basically used as means to attain medical results devoid of their consents. For example, Nazi doctors carried out some of the most horrendous experiments on humans without their consents. In the Tuskegee syphilis study, stalwart healthy black males were selected for research without their consent; even when it became evident that an alternative treatment was available, they were not treated. In view of these, a number of regulations were put in place to protect vulnerable populations. For example the Declarations of Helsinki partly indicates: “Participation by individuals capable of giving informed consent as subjects in medical research must be voluntary. Although it may be appropriate to consult family members or community leaders, no individual capable of giving informed consent may be enrolled in a research study unless he or she freely agrees (article 25). Furthermore, “All medical research subjects should be given the option of being informed about the general outcome and results of the study” (article 26 paragraph 3).
These regulations stipulate that informed consent or if possible, proxy consent, must be obtained either through written, oral, or through culturally appropriate means. It seems to me that RCT could be a recipe for violating the rights and the autonomy of patients/subjects if proper consent is not obtained. It is the contention of this piece that researchers should obtain full informed consent (orally, proxy, written) from their subjects prior to conducting clinical trials especially as applicable to developing and emerging countries in the midst of equipoise. The protocol should be approved by IRB's both locally and internationally. For example, in the wake of the HIV-AIDS pandemic, a research was carried out in Kenya (between 1992 and1998) that examined the rate of mortality and morbidity for breast-fed and formula-fed infants by lactating mothers. Researchers used RCT to conduct this research, in which lactating HIV and AIDS infected mothers were clinically randomized for trial. Some were asked to only breast-feed their infants until they reach two years of age, while others were given the options of baby formula to feed their infants for two years in order to compare and ascertain the rate of transmission of HIV-AIDS from mother to child. The researchers concluded that:
"...the estimated risk of breast milk transmission of human immunodeficiency virus type 1 (HIV-1) was 16%. Forty-four percent of all HIV-1 infections among those in the breastfeeding arm were attributable to breastfeeding. This result, in conjunction with results from clinical trials of short-course antiretroviral that have reported approximately 40% to 50% reductions in perinatal transmission rates, suggest that it may be possible to reduce substantially mother-to-child transmission of HIV-1 in the developing world with interventions of moderate cost".[9]
I find this troubling because the mode of transmission of HIV and AIDS was already known and there were medical data suggesting that antiretroviral drugs prevented infant-mother transmission of HIV and AIDS. Should researchers not have truncated the research and instead focus on educating subjects about the dangers of breasts milk transmission of HIV and AIDS? Was RCT needed given all the data prior to the research? The researchers could not have argued for equipoise because an antiretroviral drug was already available and known to reduce the transmission of HIV and AIDS. I believe the researchers were partly culpable in allowing their subjects (vulnerable subjects -infants) to be exposed to a disease that was known to eventually lead to death. It is very difficult to infer any justification for the research since this particular randomized clinical trial exposed them (the human subjects) to potential and actual harm. I find this randomized clinical trial diametrically incongruous to the principle of beneficence.
CONCLUSION
Clinical research remains at the epicenter of healthcare and pharmaceutical development in our time. Historical precedents have demonstrated that even though there have been many guidelines in protecting human subjects, researchers have not always adhered to these. In particular, a situation arises in clinical research, when there are no known definitive clinical interventions/treatments and/or there are genuine uncertainties either in the mind of the researcher or within the expert community about the result of competing interventions or therapeutic procedure. Equipoise then becomes the rationale for randomized clinical trials ostensibly to compare data and determine which intervention is the best. However, as noted above, there are many ethical issues involving the use of randomized clinical trials such as the issue of informed consent and protection of vulnerable human subjects, especially in regards to populations in developing countries. This paper has argued that clinical trials should only be conducted if equipoise is tripartite; that is, if the magnitude of the doubts is ascertained by the investigator, the expert community, and the community/research subjects, and confirmed by an IRB and international review boards. Such transparency will prevent surreptitious clinical trials and protect both researchers and human subjects and ensure the highest ethical standards.
REFERENCE NOTES
[1] www.fda.gov/clinicaltrials
[2]Salim Daya Clinical Equipoise in Evidence-based Obstetrics and Gynecology (2004) 6,1^2
[3] Freedman B. Equipoise And The Ethics Of Clinical Research in New England Journal of Medicine 1987: 317: 141-145. See also Freedman B, Weijer C, Glass KC. Placebo orthodoxy in clinical research I: empirical and methodological myths. in Journal of Law, Medicine and Ethics 1996; 24: 243-251; Weijer C. Thinking clearly about research risk: implications of the work of Benjamin Freedman. IRB: A Review of Human Subjects Research 1999; 21(6): 1-5 and Fried, C, Medical Experimentation: Personal Integrity and Social Research, New York, American Elsevier, 1974. See also, Prof. Robert Klitzman, MD Lecture Notes, Global Ethics, Spring 2014; Columbia University, New York.
[4] Robert J. Hoffman MD et al Ethics, equipoise, and evidence: when should investigators decide to not test their hypothesis in American Journal of Emergency Medicine (2009) 27, 983–98; see also Scott Gelfand Clinical Equipoise: Actual Or Hypothetical Disagreement? in Journal of Medicine and Philosophy, (July 22, 2013)38: 590–604, 2013
[5] Fehintola FA et al in .J Infect Chemother. 2008 Jun;14(3):188-94. doi: 10.1007/s10156-008-0603-6. Epub 2008 Jun 24
[6] Ibid.
[7] Kremsner PG et al in Am J Trop Med Hyg. 1993 Nov;49(5):650-4
[8] Ibid.
[9] Dorothy Mbori-Ngacha et al in JAMA. 2001;286(19):2413-2420