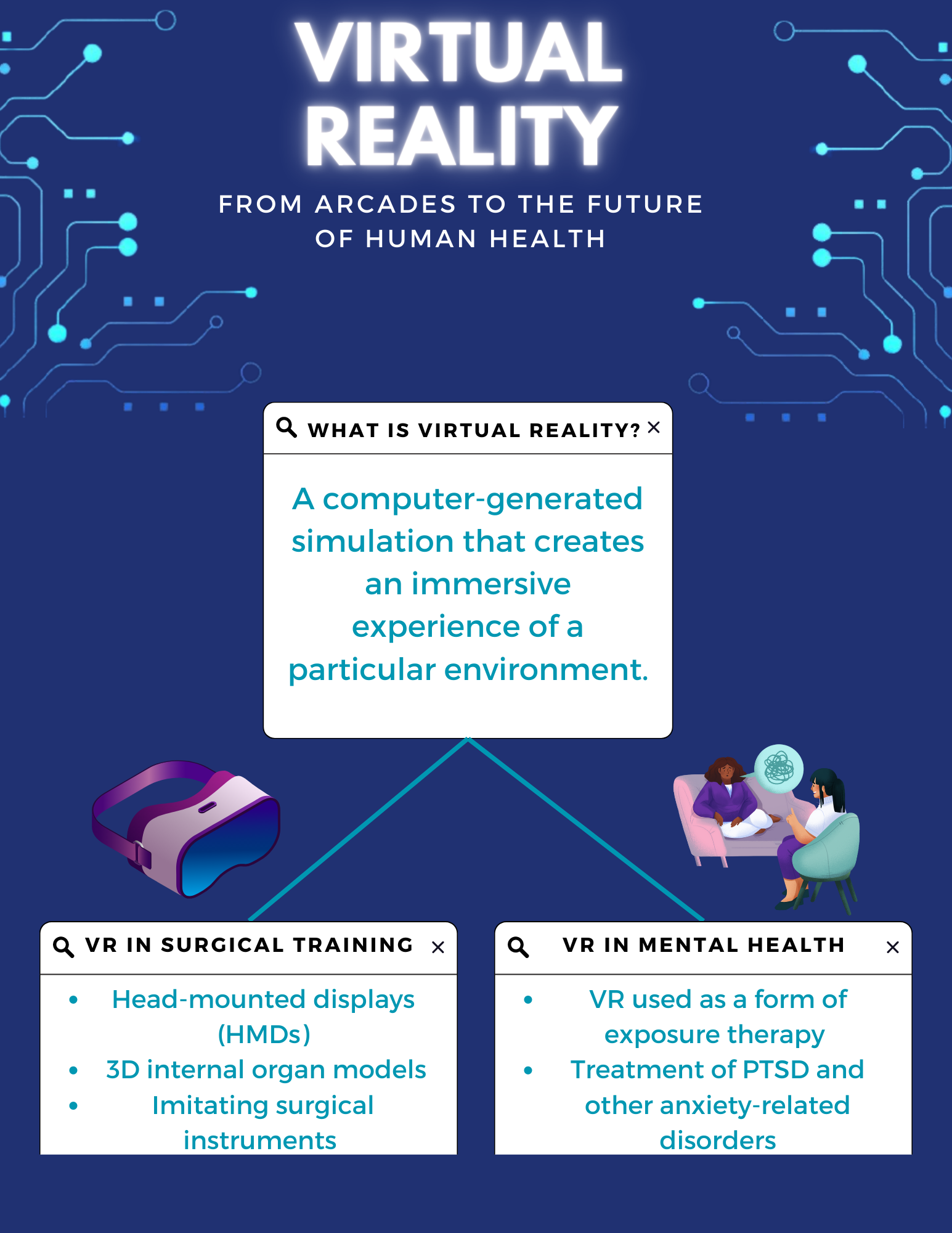
What is Virtual Reality?
A stereoscopic lens positions thousands of pixels between you and an imagined reality. While standing still, you suddenly feel the excitement of going on a roller coaster or the fright of fighting zombies in an apocalypse. These wild experiences can be encapsulated in one piece of technology: virtual reality (VR). Although virtual reality is often found in local arcades, its capacity extends far beyond that. From treating mental health conditions to aiding surgical education, virtual reality possesses immense potential in the world of medicine.
Applications of VR in Surgical Training
Considering the reduction in training hours, the availability of mentors, and the technical issues with operating systems, VR is a favorable tool in surgical training. VR simulators are combined with head-mounted displays (HMDs) to integrate surgical education and the construction of 3D internal organ models into an engaging user experience. With controllers, like joysticks, usually containing a form of communication called haptic feedback, VR controllers can precisely mimic surgical instruments. Haptic feedback can be described as controlled vibrations that occur at specific frequencies.
While this technology may sound effective in theory, many wonder if it has ever been tested during real surgical training. In one study, 53 surgeons utilized the Lap Mentor, a VR model built for removing or repairing parts of the colon during laparoscopic colectomies (Shanmugan et al., 2014). The results demonstrated that the VR tool was successful for procedure-specific metrics of the surgery. These metrics consisted of the number of movements the surgeons performed and the time it took for them to perform these movements. Another type of VR model, LapSim, enhanced training by measuring more variables, such as the depth of incision, the number of ripped and burned vessels, and the time spent performing tasks per hand (Ntakakis et al., 2023).
Applications of VR in Mental Health
In addition to surgical training, VR extends its use to mental health conditions. A traditional approach to treating mental health conditions, specifically those revolving around anxiety and fear, is exposure therapy, which involves the presence of a triggering source. However, the procedure is heavily dependent on the patient’s ability to visualize the feared stimuli, a task that isn’t quite simple to accomplish for a recovering patient. VR eliminates this barrier by creating the feared stimuli in 3D. One significant benefit of VR’s application to exposure therapy is that it can all be controlled in a clinical setting. The computer-generated environment can be tailored to the patient’s needs, such as using large text and minimizing distractions.
Many scientists have studied the benefits of using VR as a form of exposure therapy. One specific study focused on how VR can be used as exposure therapy for patients with post-traumatic stress disorder (PTSD). VRET, Virtual Reality Exposure Therapy, was used by six individuals with PTSD symptoms following a road accident (Beck et al., 2007). After ten full sessions of real-time driving scenarios, patients showed significant reductions in PTSD symptoms, such as avoidance and emotional numbing. Further studies related to phobias underline the significance of these breakthroughs. When offered VR exposure, only 5 of the 150 patients turned down the treatment, a much lower rate than the traditional method of exposure (Maples-Keller et al., 2017).
Limitations and Future Steps
While VR is not the sole solution, it certainly serves as a starting point for more effective medical treatments. Like many other modern advancements of our time, VR comes with various limitations. Even though purchasing the physical VR set is relatively inexpensive for medical institutions, costing under 500 dollars, which is standard for medical equipment, programming the hardware could be costly for hospital administration and users (Halbig et al., 2022). Another limiting factor arises from the reduction of face-to-face communication (Baniasadi et al., 2020). For example, in surgical training, students are often taught by in-person mentors. However, the shift to VR training may conflict with the learning style that students are already familiar with.
Despite these challenges, VR has proven to be effective in many fields of medicine. Originally created to cater to the entertainment industry and subsequently transformed to serve the future of human health, VR promotes innovation and problem-solving. Soon enough, VR may become a permanent fixture in clinical environments, fundamentally changing the direction of medicine.
References
Baniasadi, T., Ayyoubzadeh, S. M., & Mohammadzadeh, N. (2020). Challenges and practical considerations in applying virtual reality in medical education and treatment. Oman Medical Journal, 35(3). https://doi.org/10.5001/omj.2020.43
Beck, J. G., Palyo, S. A., Winer, E. H., Schwagler, B. E., & Ang, E. J. (2007). Virtual reality exposure therapy for PTSD symptoms after a road accident: An uncontrolled case series. Behavior Therapy, 38(1), 39–48. https://doi.org/10.1016/j.beth.2006.04.001
Bell, I. H., Nicholas, J., Alvarez-Jimenez, M., Thompson, A., & Valmaggia, L. (2020). Virtual reality as a clinical tool in Mental Health Research and Practice. Dialogues in Clinical Neuroscience, 22(2), 169–177. https://doi.org/10.31887/dcns.2020.22.2/lvalmaggia
Halbig, A., Babu, S. K., Gatter, S., Latoschik, M. E., Brukamp, K., & von Mammen, S. (2022). Opportunities and challenges of virtual reality in healthcare – a domain experts inquiry. Frontiers in Virtual Reality, 3. https://doi.org/10.3389/frvir.2022.837616
Maples-Keller, J. L., Bunnell, B. E., Kim, S.-J., & Rothbaum, B. O. (2017). The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harvard Review of Psychiatry, 25(3), 103–113. https://doi.org/10.1097/hrp.0000000000000138
Ntakakis, G., Plomariti, C., Frantzidis, C., Antoniou, P. E., Bamidis, P. D., & Tsoulfas, G. (2023). Exploring the use of virtual reality in surgical education. World Journal of Transplantation, 13(2), 36–43. https://doi.org/10.5500/wjt.v13.i2.36
Shanmugan, S., Leblanc, F., Senagore, A. J., Ellis, C. N., Stein, S. L., Khan, S., Delaney, C. P., & Champagne, B. J. (2014). Virtual reality simulator training for laparoscopic colectomy. Diseases of the Colon & Rectum, 57(2), 210–214. https://doi.org/10.1097/dcr.0000000000000031
