Affecting over 8 million people worldwide, Parkinson’s disease is a complex neurodegenerative condition resulting in a devastating impact on motor function and quality of life (World Health Organization, 2022). The common symptoms of stiffness, muscle tremors, and difficulty speaking are caused by the impairment or death of dopaminergic neurons in an area of the brain called the basal ganglia. These neurons produce a chemical called dopamine, which is commonly known as one of the “happy hormones'' associated with pleasure, motivation, and learning, as well as movement and attention. While the exact cause of Parkinson’s disease is still uncertain, the subsequent lack of dopamine in the brain is what researchers are working to restore.
Although there is no cure, the symptoms of Parkinson’s disease can be managed using a variety of treatments including oral medication, physical therapy, and deep brain stimulation. One of the newest and most promising treatments for Parkinson’s disease is stem cell therapy, a surgical procedure that replaces unhealthy dopaminergic neurons in the patient’s brain with reprogrammed stem cells. Stem cells that reside in embryos, or fertilized eggs, have the ability to develop into any cell type in the human body, whereas adult stem cells found in the skin, fat, and blood are more specialized and develop into cell types specific to the location in which they reside. However, adult stem cells can be reprogrammed to develop into any cell of the body by inserting four specific genes into the DNA in the laboratory, creating induced pluripotent stem cells (iPSCs). This process allows scientists to transform skin stem cells into neurons, expanding the opportunities to study this disease in the laboratory.
One of the advantages of stem cell therapy for Parkinson’s disease is that these stem-cell-derived dopaminergic neurons can be placed directly into the brain and fulfill the function of the impaired neurons. As Dr. Malin Parmar, a professor and scientist at Lund University, explains “after transplantation, [the dopamine-producing neurons] connect up with the neurons in the brain so they release dopamine only when it’s needed, so that the dose and the level [of dopamine] is physiological” (Parmar, 2023) compared to oral medication for Parkinson’s disease. The goal of stem cell therapy extends beyond addressing the patient’s symptoms but rather aims to restore the function of dopaminergic neurons lost due to this disease with a targeted approach tailored to each patient.
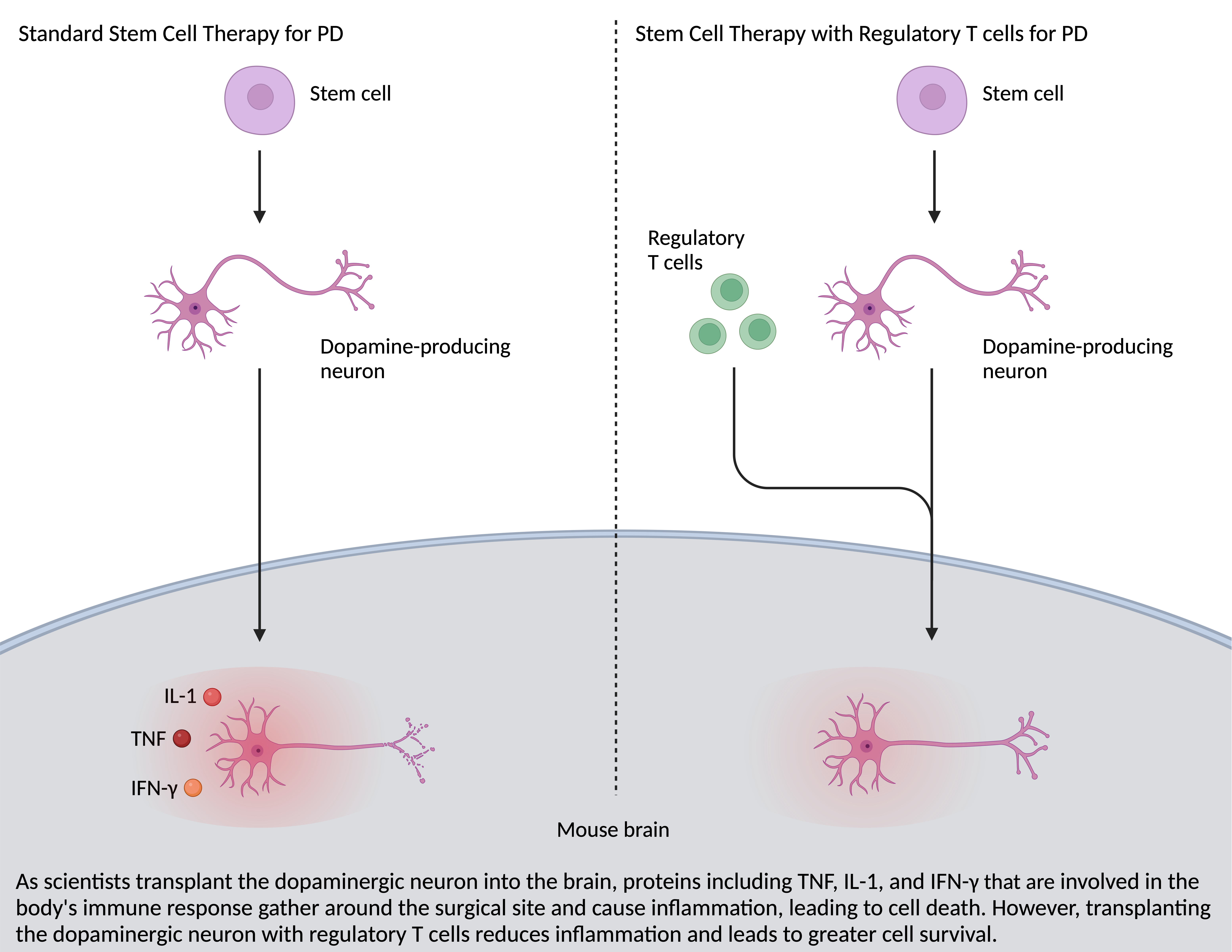
Personalized stem cell therapy for Parkinson’s disease has been tested in clinical trials since 2018, when researchers used blood cells to create dopaminergic neurons, which were then transplanted into the brain of a patient with Parkinson’s disease (Burke, 2018). However, poor cell survival and immune rejections serve as barriers that limit the incredible potential of these cell therapies. Similar to situations of traumatic brain injury, the surgical procedure of implanting dopaminergic neurons triggers an innate immune response and causes inflammation in the brain. This creates a toxic environment that has led to the death of more than 90% of the transplanted dopaminergic neurons within 2 weeks of implantation (Park, 2023).
Recently, a team of physicians and scientists from Harvard Medical School, Massachusetts General Hospital, and McLean Hospital found a way to improve dopaminergic neuron survival by combining the versatility of stem cells with the power of the human immune system. Dr. Park and his colleagues used a humanized mouse model in which stem cells from a patient with Parkinson’s disease were transferred into a mouse, which gave rise to a human-like immune system within the animal. Next, scientists created midbrain dopamine-producing neurons (mDANs) by taking skin biopsies from patients with Parkinson’s disease and implementing the right mix of chemicals and genetic modifications over the course of 28 days. The mDANs were then co-transplanted into the basal ganglia of the mouse along with regulatory T cells taken from the same patient. Regulatory T cells are white blood cells that control the body’s immune response to foreign substances within the body by suppressing other cells in the immune system (Vignali, 2008). By regulating the immune response triggered by the surgical procedure, the researchers found a significant increase in transplanted-cell survival, and a suppression of acute neuroinflammation and immune cell infiltration to the surgical site.
As the fight against Parkinson’s disease continues, Dr. Park and his team are the first to pair the power of regulatory T cells with stem cell therapy to improve dopaminergic neuron survival in cases of Parkinson’s disease. Beyond its implications for Parkinson’s disease, these findings advance innovative therapeutic strategies for other neurodegenerative conditions like Alzheimer’s disease, amyotrophic lateral sclerosis (ALS), and Huntington’s disease. While this technique requires further research and testing before proceeding to clinical trials, it holds the potential to address symptoms of Parkinson’s disease using a personalized approach and improve quality of life for millions of patients.
References
Burke, Chelsea Weidman. (2018, August 10). World’s first clinical trial to treat Parkinson’s disease with stem cells. Science in the News at Harvard University. https://sitn.hms.harvard.edu/flash/2018/worlds-first-clinical-trial-treat-parkinsons-disease-stem-cells/.
Park, TY., Jeon, J., Lee, N. et al. (2023, July 12). Co-transplantation of autologous Treg cells in a cell therapy for Parkinson’s disease. Nature 619, 606–615. https://doi.org/10.1038/s41586-023-06300-4
Parmar, Malin. (2023, July 11). Stem cell (dopamine cell replacement) therapies for Parkinson’s. Cure Parkinson’s. https://cureparkinsons.org.uk/research/curing-parkinsons/stem-cell-treatment/.
Vignali, D. A., Collison, L. W., & Workman, C. J. (2008). How regulatory T cells work. Nature reviews. Immunology, 8(7), 523–532. https://doi.org/10.1038/nri2343
World Health Organization. (2022, June 14). Launch of WHO's Parkinson disease technical brief. https://www.who.int/news/item/14-06-2022-launch-of-who-s-parkinson-disease-technical-brief#:~:text=Globally%2C%20the%20prevalence%20of%20Parkinson,for%20any%20other%20neurological%20disorder.
