On average, a person swallows 500-700 times per day. However, the quality of these swallows differs from person to person.
By many, the act of swallowing is considered a mere instinct; however, researchers and clinicians at Northwestern University’s Swallowing Cross-Systems Collaborative (SCSC) Laboratory work to rehabilitate this skill in patients experiencing dysphagia, which manifests in aspiration and atypical respiratory swallow coordination.
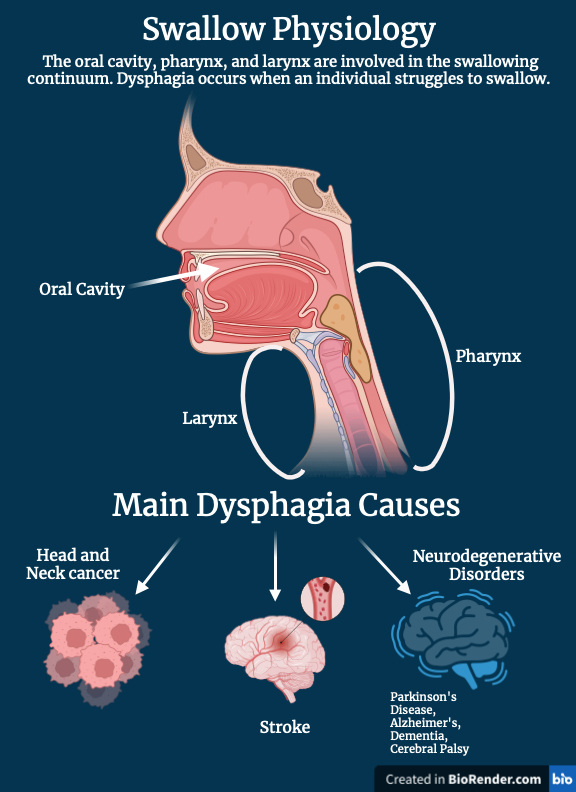
For many, swallowing is a thoughtless act requiring little to no effort. However, researchers report that deglutition—or swallowing—is a continuum that uses muscle groups from the mouth, specifically the oral cavity, pharynx, and larynx (Panara et al., 2022). Additionally, the ideal respiratory swallow coordination occurs at mid to low lung volume levels as it ensures airway protection and avoids aspiration (McFarland et al., 2016).
However, the process of swallowing differs drastically in patients with neurodegenerative disorders as their dopamine deficiency leads to trouble with efficiency of movement, affecting their ability to swallow at mid-low lung volumes (Valencia et al., 2021). Neurologic disorders resulting in oropharyngeal dysphagia include cerebral palsy, stroke, muscular dystrophy, myotonic dystrophy, and Parkinson’s Disease (PD) (Panebianco et al., 2020).
In her systematic review, Rabab Rangwala, PhD Candidate at Northwestern University, examines deficiencies in respiratory-swallow coordination in patients with Parkinson’s Disease (PD). Rangwala’s research is conducted at Northwestern University’s SCSC Laboratory, whose research indicates that post-treatment head and neck cancer patients often experience deficiencies in respiratory-swallow coordination characterized by dysphagia (Rangwala et al., 2023).
Rangwala determines that atypical respiratory-swallow coordination is a recurring symptom in individuals with PD. Additionally, Dr. Erin Reedy, post-doctoral fellow at Northwestern University, demonstrates that abnormal bolus (a swallowed substance) invasion is prevalent amongst post-lung transplant patients (Reedy et al., 2023). Reedy’s research highlights an individual’s swallow function deterioration as they endure degenerative complications. Their research proves that poor respiratory-swallow coordination manifests itself not only in patients that have undergone invasive head and neck cancer treatments or procedures, like chemoradiation or tumor resection surgeries, but also in patients with neurological disorders that are increasing in prevalence.
Indeed, dysphagia is a serious concern as it often leads to pneumonia, bronchitis, and malnutrition (Columbia University, 2023). However, a study conducted by the University of Yucatan gives us hope as they showed that oral motor skills in patients with Cerebral Palsy improve with oral motor treatment (Valencia et al., 2021). This research confirms that swallowing is a skill that can be acquired and rehabilitated.
One novel tool was developed by Northwestern’s SCSC laboratory. The tool, known as the Modified Barium Swallow Impairment profile, is the first standardized protocol used to assess swallow physiology (Martin-Harris et al., 2014). This tool guides clinicians and researchers in the development of treatments that optimize patients’ swallow function outcomes. Additionally, Purdue’s I-EaT Swallowing Research Laboratory is currently working on the development of a sensor that records an individual’s muscle movement as they swallow (Chris Adam, 2019). This data is then used by a doctor to detect and treat any disruption in the patient's respiratory-swallow coordination.
For most individuals, the hundreds of swallows per day go without a thought. But for many others, these swallows are painful and ridden with the risk of choking. These advancements allow us to hope that one day, patients will regain their ability to enjoy a meal or a mere smoothie with their loved ones without fear of aspiration. To research dysphagia is to try to better a patient’s quality of life by rehabilitating their ability to breathe and eat independently.
References
Panara, K. (2022). Physiology Swallowing. National Library of Medicine.
McFarland, D. H. (2016). Respiratory-Swallowing Coordination in Normal Subjects: Lung Volume at Swallowing Initiation. National Library of Medicine.
Widman-Valencia, M. E. (2021). Oral Motor Treatment Efficacy: Feeding and Swallowing Skills in Children with Cerebral Palsy. PubMed Central.
Panebianco, M. (2020). Dysphagia in Neurological Diseases: A Literature review. National Library of Medicine.
Rangwala, R. (2023). Respiratory-Swallow Coordination in Individuals with Parkinson’s Disease: A Systematic Review and Meta-Analysis. National Library of Medicine.
Reedy, E. L. (2023). Characterizing Swallowing Impairment in a Post-Lung Transplant Population. American Speech-Language-Hearing Association.
Columbia University Irving Medical Center (2023). Neurologic Dysphagia. Ear, Nose & Throat. NewYork-Presbyterian.
Martin-Harris, B. (2014). MBS Measurement Tool for Swallow Impairment—MBSImp: Establishing a Standard. National Library of Medicine.
Adam, C. (2019). Millions With Swallowing Problems Could be Helped Through New Wearable Device. Purdue University Research Foundation News.
