Picture this: an excruciating rollercoaster ride of hormones that comes pre-packaged with unwelcome hair growth, periods that like to play hide and seek, and an abundance of sex hormones that pave the path to potentially life-threatening diseases. The name of this rollercoaster is polycystic ovary syndrome (PCOS) and these circumstances are a fatal reality for thousands of women worldwide.
Known as one of the most common gynecologic malignancies in the world, PCOS is a common endocrine disorder that touches the lives of women from all walks of life, affecting nearly 5 million individuals in the US alone (Tabassum et al. 2021). Within the complex realm of women’s health, the question of what precisely causes PCOS has haunted endocrinologists for decades.
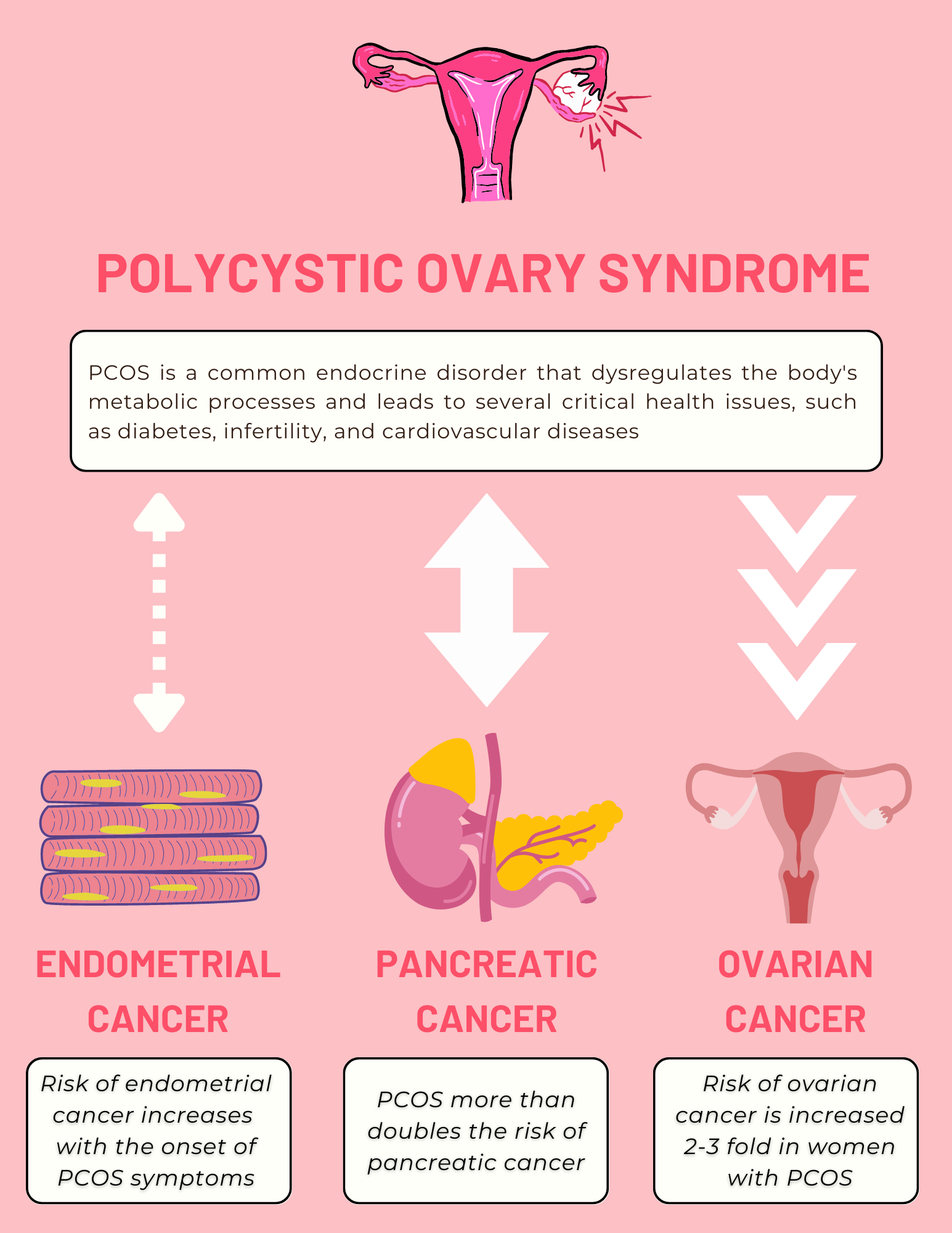
But here’s where it gets even more confusing: recent research has provided disturbing evidence that PCOS might be linked to more than just hormone imbalances. While PCOS has been known to lead to an increased risk of infertility, diabetes, and cardiovascular diseases (Daniilidis et al. 2009), medical experts have recently begun exploring the strong link between PCOS and the triad of female cancers: pancreatic, endometrial, and ovarian cancer.
First on the list is pancreatic cancer, which occurs when abnormal cells in the pancreas grow out of control; with about 62,000 cases diagnosed every year, this condition has a reputation as the 8th most common cancer in women (Peeri 2022). A study conducted at Memorial Sloan Kettering Cancer Center found that having PCOS nearly doubles a person’s risk of developing cancer (Peeri, 2022). To amplify concern, research conducted in Sweden reported that people with PCOS had a 3.4 times higher risk of developing pancreatic cancer (Peeri, 2022).
Shifting focus, endometrial cancer is a disease in which cancer cells form in the endometrium, or the lining of the womb. More than 65,000 women are diagnosed every year, with complaints of painful urination and sex (Penn Medicine). In a Taiwan-based study, 8,155 patients with PCOS were compared to 32,620 without PCOS. After following their medical diagnoses over a period of time, the researchers found that the patients with PCOS had a significantly higher risk of endometrial cancer within the first 5 years of follow-up (Ding et al. 2018).
Lastly, we turn to ovarian cancer, which is the growth of invasive cells in the ovaries, the organ that produces hormones in females. While the average lifetime chance of ovarian cancer is 1 in 78 women, PCOS increases this risk dramatically (Torre et al. 2018). A literature study conducted by the Oxford Journal of Clinical Endocrinology & Metabolism found that ovarian cancer is increased 2-3 fold in women with PCOS (Carmina & Lobo, 1999).
Each of these cancers have specific qualities that tie them together to PCOS: common gene mutations and hormonal influences (Khan et al. 2019). However, that is the limit of our current understanding.
Despite the strong evidence for the link between PCOS and these cancers, the stability of these conclusions raise controversy in academia. Medical experts voice concern over flawed research methodologies stemming from limited sample sizes and external factors such as obesity.
This confusion has led to a significant lack of discourse, leaving pivotal research questions unanswered: are there distinct subtypes of PCOS that carry varied cancer risks? How do various PCOS factors, such as the age of onset and severity of symptoms, impact cancer development? More importantly, are there specific genetic factors that could predict the progression from PCOS to these cancers?
A profound consequence lies in this uncertainty. Without intensified research efforts, mortality rates may escalate dramatically for each of these cancers (Liu et al. 2023). It is imperative that we steer towards a future that transforms the landscape of women’s health by engaging in robust research and paving the path to effective treatments that could extend a dire lifeline to countless women grappling with PCOS and the cancer triad.
References
Tabassum, F., Jyoti, C., Sinha, H. H., Dhar, K., & Akhtar, M. S. (n.d.). Impact of polycystic ovary syndrome on quality of life of women in correlation to age, basal metabolic index, education and Marriage. PLOS ONE. https://journals.plos.org/plosone/article?id=10.1371%2Fjournal.pone.0247486
Daniilidis, A., & Dinas, K. (2009, April). Long Term Health Consequences of Polycystic Ovarian Syndrome: A review analysis. Hippokratia. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2683463/
Kshetrimayum, C., Sharma, A., Mishra, V. V., & Kumar, S. (2019). Polycystic ovarian syndrome: Environmental/occupational, lifestyle factors; an overview. Journal of the Turkish German Gynecological Association, 20(4), 255–263. https://doi.org/10.4274/jtgga.galenos.2019.2018.0142
Uterine Cancer and Endometrial Cancer - Abramson Cancer Center | Penn Medicine. (n.d.). Penn Medicine - Abramson Cancer Center. https://www.pennmedicine.org/cancer/types-of-cancer/uterine-cancer-and-endometrial-cancer
Ding, D.-C., Chen, W., Wang, J.-H., & Lin, S.-Z. (2018). Association between polycystic ovarian syndrome and endometrial, ovarian, and breast cancer. Medicine, 97(39), e12608. https://doi.org/10.1097/md.0000000000012608
Mayo Clinic. (2021, August 31). Ovarian cancer - Symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/ovarian-cancer/symptoms-causes/syc-20375941
Peeri, N. C., Landicino, M. V., Saldia, C. A., Kurtz, R. C., Rolston, V. S., & Du, M. (2022). Association Between Polycystic Ovary Syndrome and Risk of Pancreatic Cancer. JAMA Oncology. https://doi.org/10.1001/jamaoncol.2022.4540
Carmina, E., & Lobo, R. A. (1999). Polycystic Ovary Syndrome (PCOS): Arguably the Most Common Endocrinopathy Is Associated with Significant Morbidity in Women. The Journal of Clinical Endocrinology & Metabolism, 84(6), 1897–1899. https://doi.org/10.1210/jcem.84.6.5803
Torre, L. A., Trabert, B., DeSantis, C. E., Miller, K. D., Samimi, G., Runowicz, C. D., Gaudet, M. M., Jemal, A., & Siegel, R. L. (2018). Ovarian cancer statistics, 2018. CA: A Cancer Journal for Clinicians, 68(4), 284–296. https://doi.org/10.3322/caac.21456
Khan, M. J., Ullah, A., & Basit, S. (2019). Genetic Basis of Polycystic Ovary Syndrome (PCOS): Current Perspectives. The Application of Clinical Genetics, Volume 12(12), 249–260. https://doi.org/10.2147/tacg.s200341
Liu, L., Habeshian, T. S., Zhang, J., Peeri, N. C., Du, M., De Vivo, I., & Setiawan, V. W. (2023). Differential trends in rising endometrial cancer incidence by age, race, and ethnicity. JNCI Cancer Spectrum, 7(1). https://doi.org/10.1093/jncics/pkad001
