In recent years, Ozempic has seen a surge in popularity. From the shining screens of Hollywood to plastered advertisements in the depths of New York City subways, Ozempic has been championed as a viral weight loss drug, promising to help users lose pounds (Smith, 2023).
So, how does Ozempic work? Glucagon-like peptide-1 (GLP-1) is a hormone produced within the body. Ozempic belongs to a class of drugs called GLP-1 agonists that mimic this hormone. When someone finishes a meal, their blood sugar levels begin to rise. In response, GLP-1 triggers an increase in the secretion of insulin, which is a hormone responsible for bringing glucose from the blood into cells. GLP-1 agonists are able to replicate the effects of GLP-1, causing a reduction in blood glucose levels (Mayo Clinic, 2022).
These drug’s ability to increase insulin secretion makes them a useful treatment for type 2 diabetes (Mayo Clinic, 2022). In patients with this condition, the body does not produce enough insulin, or the cells are not able to use this hormone (Basu, 2017). This results in high blood glucose levels, which can cause serious complications such as heart disease, eye damage, and liver damage (Cleveland Clinic, 2023a).
However, treating type 2 diabetes patients is not the driving force behind the growing popularity of GLP-1 agonists: this demand is fueled by their ability to cause weight loss (Smith, 2023). The main mechanism by which GLP-1 agonists do this is by making people feel full (Cleveland Clinic, 2023b). One way these drugs reduce appetite is by slowing gastric emptying, which is how food travels from the stomach into the small intestine. After receiving IV infusions of GLP-1, healthy participants had significantly slower levels of gastric emptying. The accumulation of food in the stomach lessens appetite, so reduced gastric emptying can cause people to eat less (Marathe et al., 2011). Another mechanism that allows GLP-1 to reduce weight is through direct interactions with neurons that determine appetite. GLP-1 reduces the activity of neurons that promote hunger and increases the activity of those that raise satiation (Shah & Vella, 2014). Due to widespread knowledge of their weight loss properties, Ozempic and other GLP-1 agonists are increasingly being prescribed to people who use them for weight loss rather than treating type 2 diabetes (Cohen, 2024). 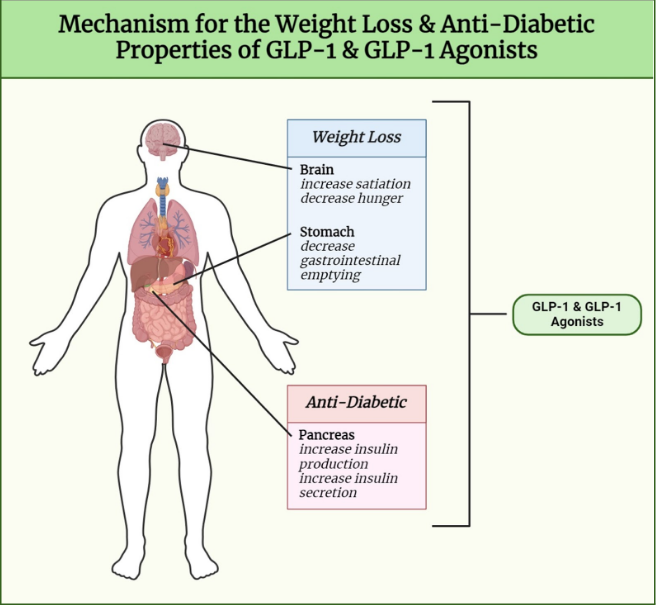
While demand for GLP-1 agonists has been increasing, the supply for these drugs has not been met with the same boost. As a result, their improper usage is causing long-term shortages, preventing people who need these treatments from getting them (Cohen, 2024). In fact, there is a current shortage of Ozempic that is expected to last until the end of 2024 (Therapeutic Goods Administration, 2024). This is especially dangerous as Ozempic and other GLP-1 agonists are long-term treatments, so lapses in their usage can be dangerous. Patients with type 2 diabetes who stop using Ozempic can face an increase in blood sugar levels and its accompanied complications (Blum, 2023).
Consequently, the drug’s meteoric rise in fame does come with a price: one that many type 2 diabetes patients cannot afford. Although Ozempic’s weight loss properties have caused it to become highly demanded, it is important that this medication is accessible to those who need it. For many patients, the use of Ozempic is not just a trend – it is a crucial treatment.
References
Basu, R. (2017, May). Type 2 diabetes. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/type-2-diabetes#:~:text=Type%202%20diabetes%2C%20the%20most,to%20be%20used%20for%20energy
Blum, D. (2023, February 3). Ozempic can cause major weight loss. What happens if you stop taking it? The New York Times. https://www.nytimes.com/2023/02/03/well/live/ozempic-wegovy-weight-loss.html
Cohen, J. (2024, July 19). Ozempic shortages raise questions about prioritizing access for diabetics. Forbes. https://www.forbes.com/sites/joshuacohen/2024/07/19/glp-1-shortages-raise-questions-about-prioritizing-access-for-diabetics/
Cleveland Clinic. (2023a, March 2). Hyperglycemia (high blood sugar). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/9815-hyperglycemia-high-blood-sugar
Cleveland Clinic. (2023b, July 3). GLP-1 agonists. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/13901-glp-1-agonists
Marathe, C. S., Rayner, C. K., Jones, K. L., & Horowitz, M. (2011). Effects of GLP-1 and incretin-based therapies on gastrointestinal motor function. Experimental Diabetes Research, 2011, 1-10. https://doi.org/10.1155/2011/279530
Mayo Clinic. (2022, June 29). GLP-1 agonists: Diabetes drugs and weight loss. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/expert-answers/byetta/faq-20057955
Shah, M., & Vella, A. (2014). Effects of GLP-1 on appetite and weight. Reviews in Endocrine and Metabolic Disorders, 15(3), 181-187. https://doi.org/10.1007/s11154-014-9289-5
Smith, S. V. (2023, April 1). 'You forget to eat': How Ozempic went from diabetes medicine to blockbuster diet drug. NPR. https://www.npr.org/2023/04/01/1166781510/ozempic-weight-loss-drug-big-business
Therapeutic Goods Administration. (2024, July 2). About the Ozempic (semaglutide) shortage 2022 - 2024. Therapeutic Goods Administration. https://www.tga.gov.au/safety/shortages/information-about-major-medicine-shortages/about-ozempic-semaglutide-shortage-2022-2024#:~:text=for%20other%20reasons.-,When%20will%20the%20Ozempic%20shortage%20end%3F,organisations%20to%20monitor%20this%20situation.
