The Push to Integrate Mid-Level Providers into Dentistry
Main Article Content
Abstract
Photo by lafayett zapata montero on Unsplash
INTRODUCTION
Mid-level providers are not new to the field of medicine. Nurse practitioners and physician assistants have been providing direct care for patients with the oversight of licensed physicians for many years. As a result of their assistance, physicians can focus on complex cases and oversee a larger patient base. This, in turn, creates a more accessible healthcare system. Although many gaps remain between medicine and dentistry, mid-level providers may be the answer to expanding access to dental healthcare needs. Recently, mid-level providers have entered the field of dentistry in multiple states in the US. People commonly refer to this role as a dental therapist. A dental therapist works under a licensed dentist providing preventive and routine restorative care to expand dental healthcare to underserved populations.[1] This new addition to the workforce has proven to be beneficial in some regions but has opened a door to ethical debate among dentists and public health officials.
In 2009 Minnesota approved the first state-wide legislation in the US to legalize the role of dental therapists after seeing a drastic decline in their dentist-to-population ratio. The congregation of dentists in high-income and highly populated areas have left many communities in the US in need of dental care but unable to receive it locally. A case study performed by dental hygienists Minnesota, from 2003 to 2007, concluded that one in four primary school children presented with visible decay, and half of these cases were deemed urgent due to symptoms including toothaches and other oral pain.[2] Minnesota health professionals performed another case study which presented results that they believed to further strengthen the need for dental reform in the state. Over the course of a year, health professionals surveyed seven hospitals in the Minneapolis-St. Paul metropolitan area. The results showed over 10,000 emergency room visits were from dental-related problems such as abscesses or toothaches. These patients had untreated oral health problems, eventually leading to infection and unbearable pain. The total cost for these emergency room visits exceeded $4.7 million in out-of-pocket payments and insurance costs.[3] These issues surrounding dental health care are evident on a national level as well. To visualize the need for expanded oral care on a larger scale, in 2022 researchers recorded that over 69 million people in the US live in areas that have a dental health professional shortage. According to federal regulations, a shortage of providers indicates a population-to-provider ratio that meets or exceeds 5,000:1.[4]
Integrating the role of dental therapists into the healthcare system has solved similar issues elsewhere. Alaskan Native communities and countries including the UK, Canada, and New Zealand have used dental therapists for decades.[5] In recent years Maine, Oregon, Washington, Arizona, Michigan, Idaho, New Mexico, Connecticut, and Nevada joined this list.[6] As of 2022, there are five dental therapy licensing programs in the US, located in Alaska, Washington and Minnesota. Dental therapists are required to have a bachelor’s degree in dental therapy and can pursue a master’s in dental therapy to extend their license and perform more advanced procedures.[7] Differences in education, allowed procedures, and state-specific requirements in Minnesota are depicted in Table 1 (state-to-state specifics may vary).
Table 1: The Varying Degrees of Dental Therapy
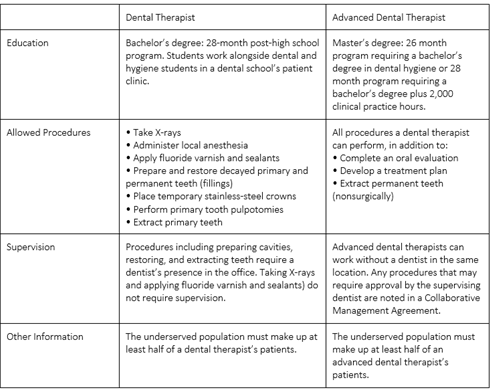
*State of Minnesota, Minnesota Administrative Rules, 150A.105, https://www.revisor.mn.gov/ statutes/?id=150a.105; State of Minnesota, Minnesota Session Laws (2009), Regular Session, Chapter 95—S.F. No. 2083, http://www.dentalboard.state.mn.us/Portals/3/Licensing/Dental%20Therapist/DTLEG.pdf; and Minnesota Board of Dentistry, “Dental Therapist Scope of Practice,” http://www.dentalboard.state.mn.us/Portals/3/Licensing/Dental%20 Therapist/DTSCOPE.pdf.
I. Regional Outcomes of Employing Dental Therapists
The goal of integrating dental therapists was to increase access to care in underserved areas. Results from a 2017 data collection on dental therapists in Alaska provide evidence that the region met this goal. Residents in communities where dental therapists practiced presented with more restorative care and fewer extractions than in communities without.[8] Another statistic reported an increase in private practices opening their doors to Medicaid patients after the addition of a dental therapist to their team. One practice recorded that their dental therapist treated over 200 Medicaid patients and earned nearly $24,000 in additional profit for the practice that year.[9] Expanding dental care to patients enrolled in Medicaid programs has been an ongoing issue. According to the American Dental Association, in 2018, around 30 percent of practicing dentists accepted Medicaid.
In 2012, a case study was conducted in Alaska, which collected the statistics produced by Rochelle Furry, a certified dental therapist. Over the course of a year, Furry saw 750 patients and performed 5,000 procedures. Furry’s addition to the team cost the supervising dentist $180,009 in overhead. Furry’s collections totaled $385,338, with a yearly net profit of $205,329.[10] Another benefit reported by dentists when integrating a dental therapist into their team was the ability to prioritize their focus toward more complex cases, leaving routine fillings and other minimally invasive procedures in the hands of the dental therapist. With the reduced education of dental therapists comes reduced costs per procedure. This may encourage patients who are uninsured or owe out-of-pocket payments and entice them to follow through with the diagnosed treatment.
II. Areas of Debate
Despite providing benefits to patients and supervising dentists, dental therapists are not prevalent throughout the US. Similar to the debate regarding mid-level providers like physician’s assistants and nurse practitioners, there are disputes between healthcare officials on whether the addition of dental therapists is an ethical solution to the disparities in access to oral care. The different levels of education between dentists and dental therapists spark debates on whether dental therapists have enough training to treat patients. Dentists are required to complete both a bachelor’s and a doctorate program, as well as pass rigorous board exams usually totaling eight years of additional education after a high-school degree. Although dental therapists perform more routine procedures that are minimally invasive, they are primarily working with populations that have received minimal oral care in the past, usually presenting with larger amounts of decay. This increases the complexity of cases that a healthcare worker with minimal training compared to a DDS or DMD attends to. While some patients prefer the low costs of procedures done by a dental therapist, others prioritize quality of treatment and believe only dentists are well-trained enough to provide it. Some argue that a doctorate-level medical professional should do irreversible procedures involving the permanent removal of the tooth surfaces, such as fillings, crowns, or extractions. This position also brings up the issue of a two-tiered healthcare system in which patients of low socioeconomic status are treated by providers with less training, while mid to upper class patients are treated by doctors. Some public health professionals argue there are better solutions. For example, the Academy of General Dentistry “White Paper on Increasing Access to and Utilization of Oral Health Care Services" suggests that one of the biggest challenges in achieving optimal oral health for all is “underutilization of available oral health care.”[11] This argument addresses the noneconomic barriers in seeking professional care, including the patient's behavioral factors, levels of oral health literacy, transportation, location, and cultural or linguistic preferences. This author concludes that increased access can be achieved with the current dentist supply, if optimally utilized, along with public health officials increasing public knowledge and awareness regarding oral health.[12]
CONCLUSION
The remaining question is what may be the best way forward for the health of the US population. The goal of equal and accessible healthcare is not easily obtainable. The introduction of dental therapists to the workforce has provided a possible solution to this problem by expanding access to healthcare to affected populations. Some regions have documented benefits from this addition, but disagreements remain among healthcare professionals on whether this is the ethical solution to the problem of oral health disparities. The practice of integrating dental therapists into all regions with oral health care shortages throughout the US comes down to whether licensed dental therapists are competent in rendering quality treatment in underserved areas. Some are content with the addition of dental therapists, while others continue to look for other solutions, such as better dental education on prevention and optimizing access to already established practices.
-
[1] Corr, Allison. “What Are Dental Therapists?” The Pew Charitable Trusts, The Pew Charitable Trusts, 9 Oct. 2019, www.pewtrusts.org/en/research-and-analysis/articles/2019/10/09/what-are-dental-therapists.
[2] The Pew Center on the States. “The State of Children’s Dental Health: Making Coverage Matter.” Pew Children’s Dental Campaign, Sept. 2010. https://www.pewtrusts.org/~/media/legacy/uploadedfiles/wwwpewtrustsorg/reports/state_policy/childrensdental50statereport2011pdf.pdf.
[3] Pew Center on the States (2010).
[4] Health Workforce Shortage Areas, Health Resources and Services Administration (HRSA), 31 Mar. 2023, https://data.hrsa.gov/topics/health-workforce/shortage-areas.
[5] David A. Nash, Jay W. Friedman, Kavita R. Mathu-Muju, Peter G. Robinson, Julie Satur, Susan Moffat, Rosemary Kardos, Edward C.M. Lo, Anthony H.H. Wong, Nasruddin Jaafar, Jos van den Heuvel, Prathip Phantumvanit, Eu Oy Chu, Rahul Naidu, Lesley Naidoo, Irvi. “A Review of the Global Literature on Dental Therapists.” Community Dentistry and Oral EpidemiologyVolume 42, Issue 1 p. 1-10, Wiley Library Online, 3 May 2013, https://doi.org/10.1111/cdoe.12052.
[6] Corr (2019).
[7] Urahn, S. and Schuler, A. (2014) Expanding the Dental Team. The Pew Charitable Trust. https://www.pewtrusts.org/-/media/assets/2014/06/27/expanding_dental_case_studies_report.pdf
[8] Corr (2019).
[9] Corr (2019).
[10] Nash, et al. (2013).
[11] White Paper on Increasing Access to and Utilization of Oral Health Care Services, Academy of General Dentistry, July 2008, https://www.agd.org/docs/default-source/advocacy-papers/agd-white-paper-increasing-access-to-and-utilization-of-oral-health-care-services.pdf?sfvrsn=2%20.
[12] Burton L. Edelstein, DDS, MPH. “Examining Whether Dental Therapists Constitute a Disruptive Innovation in US Dentistry.” American Journal of Public Health, American Public Health Association, Oct. 2011, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3222362/.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.

