Not Just Non-Consensual Pelvic Exams The Need for Expressed Consent for All Intimate Tasks for Elective Procedures
Main Article Content
Abstract
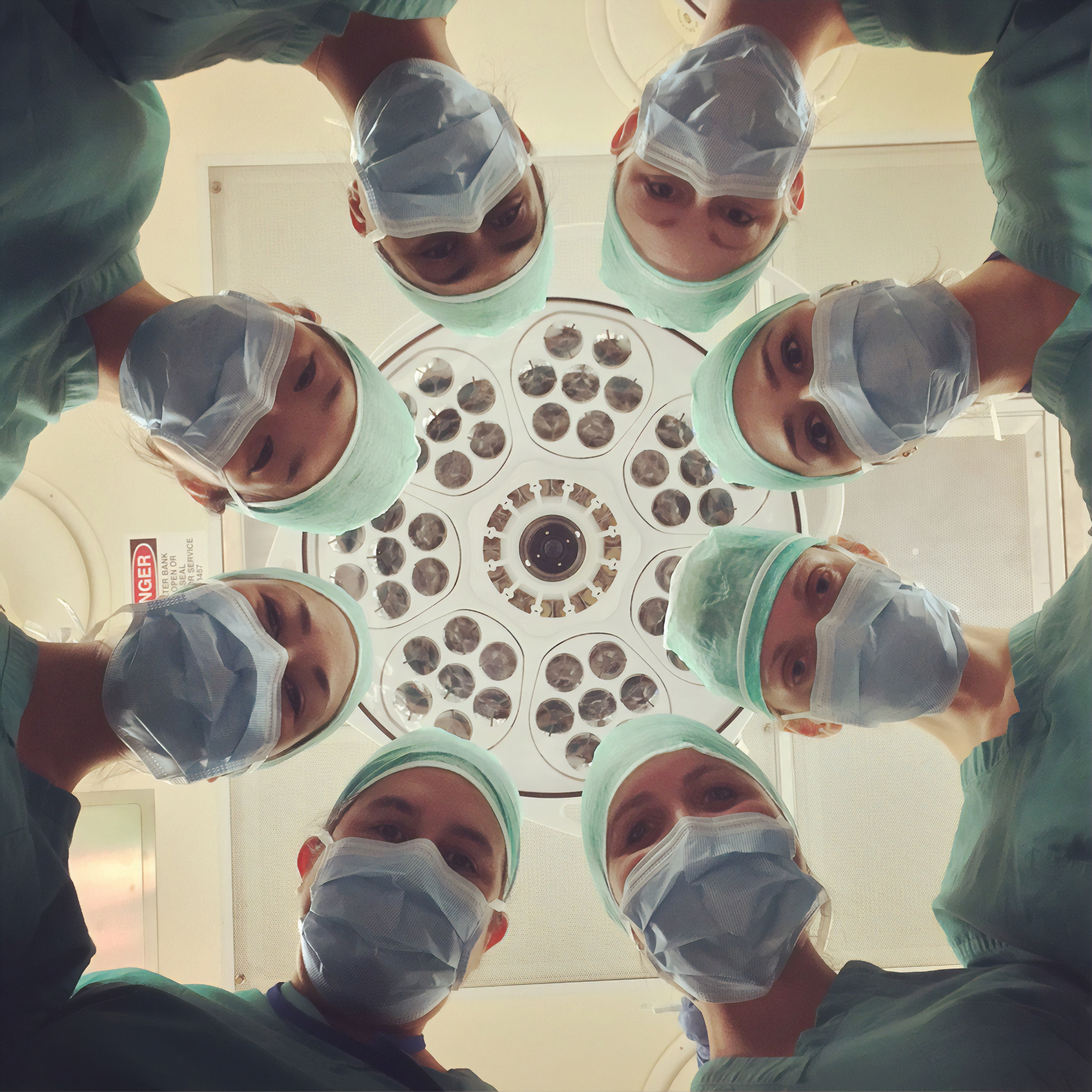
Photo by National Cancer Institute on Unsplash
ABSTRACT
Medical professionals sometimes perform intimate tasks while prepping patients for surgical procedures. These tasks may include urinary catheterization, underwear or gown removal, pubic hair removal, and groin sanitization. The intimate nature of these tasks calls for informed consent. Performed without consent, these intimate functions can result in long-term psychological harm. Given the parallels in the arguments for regulating unauthorized sensitive exams, like pelvic exams under anesthesia, policymakers and legislators should expand their efforts to require express consent for all intimate encounters that occur before, during, and after elective medical procedures to protect all patients.
INTRODUCTION
Healthcare facilities should be safe places where individuals seek healing without fear of assault on their personal dignity, bodily sanctity, autonomy, and humanity. Patients who have undergone non-consensual pelvic, rectal, prostate, and other sensitive exams and procedures – whether for diagnostic or educational purposes – have discovered that this is not always the case after emerging from the experience with a sense of violation and betrayal. Proponents of requiring explicit consent for these invasive exams have likened them to sexual abuse, which disempowers, humiliates, and degrades victims, resulting in long-lasting psychological harm. However, these sensitive exams and procedures are not the only sources of traumatic, unauthorized intimate experiences in medical settings. Indeed, both male and female patients who have endured urinary catheterization, underwear or gown removal that resulted in intimate exposure, pubic hair removal, groin sanitization, and other such intimately invasive preparatory practices without their knowledge or explicit consent have expressed the same sense of bodily violation and psychological harm as patients who have undergone non-consensual sensitive exams. While some patients have no concern over these invasive ancillary procedures, others take issue with medical staff manipulating their private spaces without express consent. This paper explores how to resolve the issues that cause harm in some patients due to nonconsensual intimate tasks associated with procedures.
I. Background
Some surgeries include prepping private areas of a patient’s body that are not directly involved in the procedure to mitigate contingencies that would require access to veins and arteries.[1] Given that physicians commonly exclude information about prep and that medical staff perform these tasks after anesthesia, some patients may be initially unaware of these intimate functions and have not provided express consent.
While the media have begun to share the accounts of individuals, mostly women, who have spoken up about their unwanted medical exams,[2] the voices of those suffering the same psychological harm after experiencing other non-consensual intimate encounters in medical settings have remained largely unheard. Yet, there are some who have shared their accounts anonymously on the website of Medical Patient Modesty (MPM), a non-profit organization that seeks to educate patients about potential privacy issues that may occur in medical settings. A survey of these accounts suggests a wide array of bodily violations. In addition to women, a significant number of men submitted their stories. The following are a few excerpts:[3]
“John” from Iowa stated that he was traumatized after discovering that staff had removed the disposable underwear they had given him and clipped his pubic hair while he was sedated for a procedure that involved incisions around his knee. He claimed that nobody ever mentioned his groin. John asserts that medical personnel deceived him into believing they were protecting his bodily privacy by providing him with disposable underwear and then removing it when he was sedated.
Jeffrey Fox from Virginia said that he suffers from PTSD as a result of a female nurse clipping his pubic hair for open heart surgery. He noted that staff instructed him not to shave his chest, implying that they would perform the task. But nobody mentioned anything about his groin.
Kevin reported that his sister sexually abused him at a young age and that he was retraumatized as an adult when he awakened from hernia surgery to discover that staff had clipped his pubic hair and inserted a urinary catheter without his knowledge or consent.
Due to anxiety as a result of trauma from an incident involving genital exposure, RM from Pennsylvania made multiple appeals to the doctor to leave his underwear on during an angiogram centering around his wrist. After the doctor denied his request, he unwillingly relented and ultimately suffered further trauma when staff clipped his pubic hair and left him exposed. RM stated that clipping his pubic hair for a procedure centering around his wrist was “completely unnecessary” and an “unforgivable violation” of his privacy.
Beth from Oklahoma submitted an account on behalf of her husband who was traumatized after awakening during hand surgery to discover that staff had stripped him naked.
“Man Who Had Carpal Tunnel Surgery” refused to remove his underwear only for staff to take them off after he had been anesthetized.
“Lynn” from Mississippi stated that she suffers from PTSD after a dermatologist lifted the waistband of her shorts, peered down, and placed his hand against her groin for the stated purpose of taking her pulse. The event occurred when she was a young girl, and she was retraumatized decades later when medical staff subjected her husband to a similar unwanted intimate encounter while he was sedated for a procedure involving his knee. She says that both she and her husband have suffered a sharp decline in their mental health as a result of their medical experiences.
Marie stated that she unsuccessfully appealed to medical staff to leave her underwear on and then was traumatized when they exposed her genitals while positioning her for knee surgery.
“Concerned human being” from Kentucky relayed the account of his wife, an RN who had expressed concerns to him over witnessing unnecessary intimate exposure of patients only to find herself on the receiving end of a dignity violation when she awoke after her procedure to fix a tendon in her finger to find staff had removed her gown and laid it across her during transport out of the OR.
These accounts are just a few of the first-hand narratives on the MPM website. I do not use them to make assumptions about the scope of the problem. Instead, this paper suggests these narratives are an important source for any advocates for changes that better respect patient dignity.
II. Consent
It is apparent that medical professionals did not inform these patients of the intimate encounters they would experience. As many attest, patients often begrudgingly remove their underwear when medical professionals instruct them to do so before procedures. Patients such as the ones from the MPM website may not understand why they must remove their underwear and may not wish to ask. Some acquiesce to the requests for underwear removal because they do not wish to reschedule a long-awaited procedure or appointment. Thus, they may experience duress after unsuccessfully appealing to leave their underwear on. While medical professionals may argue that there are medical reasons for these intimate functions, such as access to arteries, these explanations do not account for a lack of consent. Simply declaring that a task or procedure is routine and necessary does not render clinicians' actions ethical or less of a violation.[4]
Patients have a right to know if their private areas will be involved at any point during a medical experience so they can determine for themselves if these intimate procedures and tasks are reasonable. Some patients may not agree that underwear removal is essential, that clipping pubic hair and cleansing the groin is necessary, or that urinary catheters are required. Multiple patients from the website appear to share this sentiment and expressed feelings of confusion and distress over the fact that their providers had never informed them of these intimate preparatory tasks. Assuredly, they believe they never truly consented to the experiences medical staff ultimately subjected them to.
III. Informed Consent
Informed consent is a shared decision-making process by which practitioners discuss the benefits and risks of undergoing or rejecting an invasive procedure. Providers must disclose sufficient information to enable patients to make informed decisions and then document consent in a consent form.[5] Ultimately, clinicians do not know what patients find important. They document consent in a vague form that the medical community can interpret to the disadvantage of patients. But informed consent transcends a signature on a form.[6] As one bioethicist notes regarding intimate medical exams, “Clearly, standard consent forms fail to give patients the granularity they need to properly consent.”[7] I argue that consent forms should name the ancillary intimate tasks that doctors and medical staff plan to perform, especially those that patients might not expect, and when staff will conduct such tasks under anesthesia without the opportunity for patients to verbally consent at the moment. Obtaining informed consent for intimate preparatory steps should be a requirement, just as obtaining informed consent for the procedure is.
Consents are a version of waivers that patients present as right holders of their bodies for medical workers to access limited body parts for a limited amount of time.[8] When a violation of this waiver occurs, a patient’s bodily autonomy and sanctity is violated. Informed consent is the cornerstone of patients’ rights, and understanding is the cornerstone of informed consent. A patient can only understand – and consent to – a procedure as a physician explains it. Due to the knowledge asymmetry in medical settings, patients rely on the fiduciary relationship with their physician to safeguard their physical and psychological well-being. To adhere to ethical standards, medical professionals should include details about surgical prep when the tasks required are intimately invasive. For example, medical professionals should disclose tasks like removing undergarments and shaving intimate areas in advance to allow patients to ask any questions about the necessity of those tasks and then properly consent or withhold consent. Deliberately withholding information patients would find important is tantamount to lying because a deceptive person “acts in such a way that the other person can never agree with how she or he is being treated.”[9] Therefore, it is understandable – and expected – that the patients from the MPM website, like individuals who have experienced a non-consensual sensitive medical exam, could feel betrayed.
These intimate tasks involved in preparing patients for procedures should be included in the informed consent process. Some ethicists and medical professionals contend that convenience is a reason why providers exclude information about sensitive procedures and suggest that hospitals are concerned that patients would decline procedures if they were aware of ancillary sensitive exams and tasks, prompting them to change their practices.[10]
Maggie from the MPM website, who was distressed over learning that an anesthesiologist had administered an amnesiac drug and then discovered from her records that her surgical team consisted mostly of men after her provider assured her beforehand that all the staff would be female, reported that her doctor and hospital responded to her complaints with, “that's why people are sedated. Hospitals/surgeons don't want patients to know what's happening during surgery—it's not necessary. Most patients like you would just object, so sedation helps everyone.”[11] This approach is paternalistic, insulting, and harmful. Performing a procedure after choosing not to seek consent out of fear that a patient would reject it “violates the very concepts of consent, patient autonomy, and individual rights.”[12]
IV. Implied Consent
Implied consent is another reason why medical community members believe that express consent for preparatory procedures is unnecessary. They allege patients implicitly consent to these tasks when consenting to the general procedure. Implied consent assumes that the patient possesses prior knowledge and expectations that medical personnel could perform a specific task, and thus, there is a presumption of consent. Medical staff are presuming consent, yet patients may feel they have done nothing to imply consent.[13] Not all patients anticipate medical staff accessing intimate areas of their body while prepping for a non-intimate procedure.
Relying on implied consent undermines the well-documented right to refuse treatment because of the lack of information. Medical personnel deprive patients like the individuals from the MPM website of the right to determine what happens to their bodies, particularly their most private parts. Assuming that patients have implicitly consented to intimate preparatory tasks for a non-intimate procedure denies them the right to safeguard their bodily sanctity themselves and forces patients to adhere to the provider’s concept of dignity.
Relying on implied consent is an abuse of a provider's privileged position of power. Medical harm results from “not only … a physical perpetration but as an act of power of one person over another'' and that “Patients [and] family members [are] burdened…by the thoughtless and insensitive exercise of power."[14] Abusing a privileged position of power creates an intimidating and unwelcoming environment, especially for modest individuals and vulnerable members of society, such as sexual assault victims who are hyper-protective of their bodily privacy, sanctity, and autonomy.
In the context of sexual assault, “A sleeping, unconscious, or incompetent person cannot consent.”[15] Federal law, state laws, and university policies address consent, also in the context of sexual assault. For example, the University of Iowa’s sexual misconduct policy defines consent as “knowing, voluntary, and clear permission by word or unambiguous action.”[16] This provides a clear definition of consent as it applies specifically to intimate areas of the body the policy defines as “breasts, buttock, groin, or genitals.” As with sexual consent, patients must be informed of the activity to which they are consenting when they are conscious. Federal and state law, along with university policy that also governs associated teaching hospitals, do not allow implied consent regarding a patient’s private parts in the context of rape or sexual assault. I suggest that they should extend this prohibition on implied consent to medicine, with the exception of emergency situations.
Federal and state laws criminalize non-consensual sexual contact either directly or through clothing with intimate areas of the body, specifically the “anus, groin, breast, inner thigh, or buttocks.”[17] Medical professionals would not generally view pre-surgical hair clipping and gown and undergarment removal as sexual in nature. Yet some patients feel otherwise. This paper highlights their perspective rather than assessing the reasonableness of their feelings. I argue that informed consent would protect individuals like those who reported being personally harmed by nonconsensual intimate contact ancillary to medical procedures.
Some patients do not think of their private areas in a detached or neutral manner.[18] For example, outside the medical context, research suggests that individuals equate clipping pubic hair to sexual activity.[19] One might argue that in the medical context, the patient may feel hair removal has a sexual aspect, and its removal is a violation. Hair removal is an example of the inability of medical practice to “abstract itself from the culture in which it operates.”[20] Providers cannot expect or force a sudden paradigm shift in how patients view and value their intimate boundaries simply because they enter a medical environment.
V. Patient Psychological Harm
Malicious intent does not have to be present for a medical professional to inflict damage given that that medical harm is “not necessarily the intention, but the byproduct of action.”[21] The patient narratives cited on the MPM website describe various harms that patients experienced due to ancillary medical tasks that involved exposing or touching intimate body parts for non-intimate procedures. In a study of women undergoing gynecological procedures, a “lack of information given to the patient…and a lack of clearly understood consent” led some women to develop PTSD.[22] I assert that these nonconsensual ancillary tasks evoke similar reactions.
Multiple patients from the MPM website expressed feelings of humiliation, embarrassment, and disrespect after staff exposed their genitals, clipped their pubic hair, and inserted a urinary catheter without their prior knowledge. Several patients from the MPM website stated that they had experienced some form of previous intimate violations and were retraumatized by their medical encounters. Lynn’s account, in particular, of second-hand re-traumatization via her husband’s experience illustrates that the damage caused by non-consensual intimate exposure and contact in medical settings is far-reaching.
Some argue that medical staff cannot harm the psyche of patients who are anesthetized.[23] The Association of periOperative Registered Nurses (AORN) even notes that “Our current protocol seems to be ‘what they don't know won't hurt them.’"[24] But patients have awakened naked during procedures that began with their underwear and gown on. And the patients from the MPM website relayed a sense of trauma when they learned afterward that a staff member had clipped their pubic hair or inserted a urinary catheter. A patient’s conscious state should not dictate what is ethically appropriate when it comes to viewing and contacting private areas.
Studies show that patients who feel violated after they experience nonconsensual intimate exposure and contact have strong convictions regarding their rights and values and ultimately forsake medical care as a result of their concerns.[25] The patients from the MPM website claimed they lost their faith, trust, and respect for the medical community due to their intimate medical experiences. Therefore, the frame of reference should not center around how medical professionals perceive their actions but that patients may feel that nonconsensual intimate encounters are sexual violations.[26]
VI. Discussion and Recommendations
Some have acknowledged a need to preserve patient modesty and dignity better, resulting in improvements in gown design and the development of surgical undergarments.[27] Additionally, some medical organizations have called for clipping hair only when necessary.[28] However, these improvements would be more effective if all hospitals and doctors followed more rigorous modesty protocols. For instance, providing improved gowns and surgical undergarments to patients is pointless if medical staff remove them without the patient’s knowledge, such as in the case of John. The issue is informed consent. It appears that medical professionals do not need permission to visually and physically access intimate areas of their patients’ bodies.
The medical community ignored sustained calls for explicit consent for sensitive medical exams for years.[29] Eventually, public awareness and scrutiny of the issues surrounding non-consensual pelvic, rectal, and other sensitive exams led to an increasing number of states passing laws requiring express consent for pelvic exams and other invasive actions. These and others should consider requiring express consent for all intimate functions, not just exams for the sake of uniformity and consistency. It is understandable that clinicians need to access private areas for serious medical reasons. But medical professionals should explain their rationale, include this information on consent forms, and give patients the opportunity to question their validity and consider all key aspects of a medical procedure – including intimately invasive preparatory functions – prior to consenting.
CONCLUSION
The core issue patients from the MPM website expressed is a loss of autonomy. From the viewpoint of the patients whose narratives are included on the MPM website, the nonconsensual intimate tasks related to medical procedures caused harm. Patients should be able to learn about all intimate functions that staff may perform while preparing for surgery. The patient would then determine whether to refuse the ancillary task or the entire procedure. While some argue attaining informed consent for such tasks is impractical, I suggest that it is an ethical imperative. When patients undergo intimate tasks that they did not expect, some experience significant psychological harm, sometimes exacerbated by re-traumatization.
Another effect is distrust of the medical community. Trust is the foundation of medical care. Patients must have confidence in a provider’s expertise, professionalism, communication, and procedural technique. The loss of any of these elements results in a breakdown of the doctor-patient relationship. Clinicians who touch a patient’s body without proper consent “risk violating the trust that forms the foundation of medical practice.”[30] Patients could forsake important medical care if patients cannot trust members of the medical community to abide by their personal notion of dignity, which includes respecting their intimate boundaries. The goal of this piece is to illustrate the need for explicit consent for intimate, invasive preparatory functions for the benefit of patients and providers alike.
-
[1] U.F.O. Themes, “Preoperative Skin Preparation.” Nurse Key. July 21, 2016. https://nursekey.com/preoperative-skin-preparation/.
[2] L.R. Wilson, C. Tanner, and S.L. Wong, “A New Layer of Informed Consent: Discussions and Documentation Regarding Sensitive Examinations in Surgery,” Annals of Surgery Open: Perspectives of Surgical History, Education, and Clinical Approaches 3 (1): e120, (March 2022). https://doi.org/10.1097/as9.0000000000000120.
[3] Bodily Privacy Violation Cases. Medical Patient Modesty. (2023). http://www.patientmodesty.org/modesty.aspx
[4] M. Valencia, “Providers Are Sexually Assaulting Patients — and It’s Legal,” Healthline. August 30, 2019. https://www.healthline.com/health/nonconsensual-internal-exams-sexual-assault.
[5]B. Murray, “Informed Consent: What Must a Physician Disclose to a Patient?” AMA Journal of Ethics 14 (7): 563–66, (July 2012). https://doi.org/10.1001/virtualmentor.2012.14.7.hlaw1-1207.
[6] “Quick Safety 21: Informed Consent: More than Getting a Signature,” (Updated: April 2022). Jointcommission.org. https://www.jointcommission.org/resources/news-and-multimedia/newsletters/newsletters/quick-safety/quick-safety--issue-21-informed--consent-more-than-getting-a-signature/informed-consent-more-than-getting-a-signature/.
[7] L. Bruce, “A Pot Ignored Boils on: Sustained Calls for Explicit Consent of Intimate Medical Exams.” HEC Forum: An Interdisciplinary Journal on Hospitals’ Ethical and Legal Issues 32 (2): 125–45, (March 9, 2020). https://doi.org/10.1007/s10730-020-09399-4
[8] P. Friesen, “Educational Pelvic Exams on Anesthetized Women: Why Consent Matters,” Bioethics 32 (5): 298–307, (April 23, 2018). https://doi.org/10.1111/bioe.12441.
[9] S.L. Seybold, “Not Just ‘Bodies with Vaginas’: A Kantian Defense of Pelvic Exam Consent Laws,” Bioethics 36 (9): 940–47, (September 6, 2022). https://doi.org/10.1111/bioe.13084
[10] Seybold , “Not Just Bodies with Vaginas,”Bruce, “A Pot Ignored Boils On”; Valencia, “Providers Are Sexually Assaulting Patients;” P. Hsieh, “Pelvic Exams On Anesthetized Women Without Consent: A Troubling And Outdated Practice,” Forbes. (May 14, 2018). https://www.forbes.com/sites/paulhsieh/2018/05/14/pelvic-exams-on-anesthetized-women-without-consent-a-troubling-and-outdated-practice/?sh=7f0b5bcb7846; D. S. Davis, “Pelvic Exams Performed on Anesthetized Women,” AMA Journal of Ethics 5 (5): 193–94, (May 2003). https://doi.org/10.1001/virtualmentor.2003.5.5.oped1-0305.
[11] Medical Patient Modesty, “Bodily Privacy Violation Cases,” www.patientmodesty.org/modesty.aspx
[12] Hsieh, “Pelvic Exams On Anesthetized Women Without Consent.”
[13] Robert M. Veatch “Implied, Presumed and Waived Consent: The Relative Moral Wrongs of Under- and Over-Informing,” The American Journal of Bioethics, 7:12, 39-41, (December 19, 2007). DOI: 10.1080/15265160701710253 (noting differences between implied and presumed consent)
[14] J. Shapiro, “Violence’ in Medicine: Necessary and Unnecessary, Intentional and Unintentional,” Philosophy, Ethics, and Humanities in Medicine: PEHM 13 (1), (June 11, 2018). https://doi.org/10.1186/s13010-018-0059-y.
[15] “10 U.S. Code § 920 - Art. 120. Rape and Sexual Assault Generally,” n.d. LII / Legal Information Institute. https://www.law.cornell.edu/uscode/text/10/920.
[16] “Prohibited Conduct,” n.d. Uiowa.edu. https://opsmanual.uiowa.edu/community-policies/sexual-harassment-and-sexual-misconduct/prohibited-conduct.
[17]Department of Justice, “Sexual Assault”; “18 USC 2246: Definitions for Chapter,” n.d. House.gov. https://uscode.house.gov/view.xhtml?req=(title:18%20section:2246%20edition:prelim).
[18] Bruce, “A Pot Ignored Boils On.”
[19] S. Ramsey, C. Sweeney, M. Fraser, and G. Oades, “Pubic Hair and Sexuality: A Review.” The Journal of Sexual Medicine 6 (8): 2102–10, (August 2009). https://doi.org/10.1111/j.1743-6109.2009.01307.x.
[20] Davis, “Pelvic Exams.”
[21] Shapiro, “Violence in Medicine.”
[22] J. Menage, “Post-Traumatic Stress Disorder in Women Who Have Undergone Obstetric and/or Gyneacological Procedures: A Consecutive Series of 30 Cases of PTSD,” Journal of Reproductive and Infant Psychology 11 (4): 221–28, (December 11, 2007). https://doi.org/10.1080/02646839308403222.
[23] Seybold, “Not Just Bodies with Vaginas”; Bruce, “A Pot Ignored Boils On.”
[24] D. O’Connor, “We got blasted for June's cover photo. Did we deserve it?” Outpatient Surgery. July 10, 2013. https://www.aorn.org/outpatient-surgery/article/2013-July-editors-page-another-photo-bomb
[25] M.C. Jacofsky, R. L. Auran, A. Williams, S. Mauro, and D. Sietsema, “Exposure-Related Anxiety and Improving Patient Satisfaction with Medical Undergarments during Surgery: A Randomized Controlled Trial,” The Journal of Bone and Joint Surgery. American Volume 104 (15): 1380–85, (August 3, 2022). https://doi.org/10.2106/jbjs.22.00126.
[26] Bruce, “A Pot Ignored Boils On.”
[27] Jacofsky, et. al. “Exposure-Related Anxiety”; P. Arunachalam and B. D’Souza, “Patient-Centered Hospital Gowns: A Novel Redesign of Inpatient Attire to Improve Both the Patient and Provider Experience,” Frontiers in Biomedical Devices 84815 (April 11, 2022),. V001T04A008, https://doi.org/10.1115/dmd2022-1058.
[28] C. E. Edmiston Jr, D. Leaper, S. Barnes, H. B. Johnson, M. Barnden, M. Paulson, J. L. Wolfe, K. Truitt, “Revisiting Perioperative Hair Removal Practices.” AORN Journal. (April 26, 2019), https://aornjournal.onlinelibrary.wiley.com/doi/10.1002/aorn.12662; Association of Surgical Technologists, “AST Standards of Practice for Skin Prep of the Surgical Patient,” n.d,, https://www.ast.org/uploadedFiles/Main_Site/Content/About_Us/Standard_Skin_Prep.pdf
[29] Bruce, “A Pot Ignored Boils on”
[30] Friesen, “Why Consent Matters.”
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.