Revisiting the Ethical Framework Governing Water Fluoridation and Food Fortification
Main Article Content
Abstract
Introduction
Nutrition is one of the most important aspects of preventative health, and interventions such as food fortification and water fluoridation have been implemented widely to ensure that populations are meeting key micronutrient recommendations. Food fortification is the idea of adding any one of a wide variety of micronutrients to staple foods to ensure that populations are meeting their micronutrient needs. Food fortification started with the addition of iodine to salt after discovering the relationship between iodine deficiency and goiter [1]. Other nutrients such as folate for the prevention of spinal bifida in newborns and vitamin D to prevent cancers, neurological, and cardiovascular diseases were later delivered to the public en masse via food fortification [2, 3].
Bioethics in healthcare typically governs the interaction and decision making between healthcare professionals and their patients. However, food fortification and water fluoridation seem out of scope compared to typical approaches, since there is no direct patient-clinician interaction and these interventions are delivered en masse to populations rather than individuals [3]. Because of this, views on informed consent, deception, beneficence, and non-maleficence need to be adjusted for context.
Recent papers have looked at the feasibility of adding statins (drugs which inhibit the production of cholesterol in order to prevent heart disease [4]) to public water supplies. Ginter et al. strongly suggested that statins should not be added to public water supplies as they will most likely cause detrimental health effects to those not suffering from high cholesterol or heart disease [5]. By contrast, the landmark JUPITER Trial (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin) found that statins administered to patients with normal or low cholesterol levels effectively reduced their chance of first heart attack or stroke [6]. Outside of statins, leading bioethicist Julian Savulescu has argued that drugs for cognitive enhancement can be added to our water and food supplies [7]. Both propositions, directly cite food fortification and water fluoridation programs as their predecessors, suggesting that adding statins and cognitive enhancers to water would be the “logical next step”.
These propositions on statins or cognitive enhancement build upon the unstated premise that water fluoridation and food fortification are ethical. However, this assumption must be revisited by reviewing the ethical frameworks that justify food fortification and water fluoridation programs. In this paper, we will consider whether the similarities between food fortification and water fluoridation override their differences and thus what ethical conclusions can be cross-pollinated between the two interventions. From there, we will analyze the ethical frameworks that both support and reject such public health interventions. Specifically, this paper will discuss the “known knowns” and the “known unknowns” concerning the ethics around water fluoridation and food fortification.
“Known Knowns” – Science of Water Fluoridation and Food Fortification
Food fortification can be generally defined as the practice of increasing the content of an essential micronutrient in a food with the aim of improving the nutritional quality of the food supply and provide a public health benefit with minimal risk to individual health [8]. Unlike the somewhat simplistic process of adding sodium fluoride or fluorosilicate derivatives to public water supplies, food fortification encompasses the addition of a broad range of nutrients to various foods. A few prominent examples of such nutrient interventions include folate being added to flour, iodine being added to salt, and the fortification of vitamin D in milk. Folate consumption was demonstrated to effectively prevent neural tube defects in unborn infants [9], iodine deficiency was demonstrated to cause goiter and hypothyroidism [10], while hypovitaminosis D was shown to cause osteoporosis amongst a vast range of other illnesses [11]. The diseases prevented by food fortification and water fluoridation should be taken into account when considering the necessity of these public health interventions.
On the other hand, water fluoridation is the practice of adding fluoride chemicals (sodium fluoride or fluorosilicate derivatives) to public water supplies for the purpose of preventing tooth decay and cavities [12–14]. Public Water fluoridation first began in 1951 while food fortification began in 1992 with the addition of iodine, vitamin A, and iron [2, 15]. Scientific evidence shows that water fluoridation prevents tooth decay by providing individuals with frequent and consistent contact with low levels of fluoride [16]. Public water fluoridation programs have been shown to reduce tooth decay by 25% in children and adults [17–20]. The introduction of fluoride also prevents other oral health complications such as gum pain, gum disease, and oral abscesses [21].
A key difference between water fluoridation and food fortification is the policies regulating when and how these interventions are to take place. In the public health context, we shall assume that fluoride is added solely to water (we will consider alternatives later). Water is unique in that it has other purposes for humans aside from consumption, such as for cleaning the body. For instance, in the United Kingdom, water is not considered food until it emerges from the taps [22]. This loophole allows the addition of fluoride to water supplies early on in the processing stages to be exempt from the regulations for food fortification despite the obvious intent that the fluoride added to the water is meant for human consumption [22].
When considering the fortification of milk, salt and flour, only milk can be considered a food product in all its respective stages (from raw milk through to its final bottled form). Flour is almost never consumed raw and its raw consumption as dough is strongly advised against by the Food and Drug Administration due to risk of infection [23]. Likewise, salt is almost never consumed in its pure form and instead is used as an additive to other dishes. In that sense, should folic acid addition to flour or iodization of salt be declassified as food fortification since they are not food in the most technical sense? Taking such a view is disingenuous (as is the British water loophole) as it ignores the intent of adding nutrients to food precursors: so that they may be consumed in their final stages of processing (with food, the cooked dish). Through this view, nutrients are added to the products with the intent of consumption. This intent should be the basis of ethical consideration, not the stage of nutrient delivery.
“Known Unknowns” – Ethical Analysis of Water Fluoridation and Food Fortification
To begin an ethical analysis of food fortification and water fluoridation, a thorough review of the similarities between the two processes brings several ethical questions/dilemmas to the fore. The key similarities between food fortification and water fluoridation can essentially be summarized in three general areas: intent, delivery, and consent (that is, the lack thereof).
1. Intent
From the outset, both water fluoridation and food fortification have similar medical intents: to alleviate nutritional deficiencies and their resulting complications in the general public. In this sense, both water fluoridation and food fortification are prophylactic, intended to prevent disease as opposed to treating an already existing ailment. The principles of beneficence and stewardship (the duty of public health authorities to act for the welfare of persons and the population, especially vulnerable populations) support the argument that governments have a duty to actively protect and promote the health and well-being of the population. One can argue that governments have access to an easy to use, safe, efficient and cost-effective means of reducing medical complications with water fluoridation and food fortification, and thus are effectively protecting the health of the populations. A question arises from the principle of beneficence regarding whether good intent can be applied to a broader range of drugs and diseases. Such propositions of adding medications to water supplies are not farfetched as there have already been debates regarding the addition of cholesterol-reducing statins to public water supplies [24]. These propositions, especially the one by Savulescu, build on the methods from food fortification and water fluoridation but shift the impetus from disease prevention to enhancement, posing new ethical challenges.
2. Delivery
The modes of delivery for both water fluoridation and food fortification are highly similar. They involve the modification of products that are staple foods, and are therefore commonly ingested. The way fluoride is delivered makes consuming fluoridated water or micronutrient-fortified foods unlike taking fluoride or micronutrient supplements, in that consumption of the supplements implies the intent of the consumer to alleviate or prevent a particular micronutrient deficiency. However, consuming fluoridated water or folate-fortified flour products does not necessarily come with this same definite intent of disease prevention on the end of the consumer. Equally, due to cost or unavailable alternatives, it may be difficult for individuals who do not wish to consume fortified foods or fluoridated water to purchase salt, flour, milk or water that do not contain these additives.
In addition to this, the consumption of fortified foods and fluoridated water are personal and do not require the direct supervision or administration of a physician or other healthcare professional. This is contrary to vaccinations (another prophylactic public health intervention) which are delivered by a healthcare provider. This also poses additional ethical questions, namely those of whether beneficence supersedes consent and whether interventions that are intended to treat populations en masse need to follow the same guidelines that govern typical medical practice.
3. Consent
The similarity in the consent procedure behind food fortification and water fluoridation is the most important area for ethical analysis. Since a healthcare provider is not administering or prescribing fluoridated water or fortified food products, there is no room for an informed express consent procedure. What makes food fortification and water fluoridation more similar to one another and different from vaccinations and nutrient supplements is the fact that there is an implicit deception involved with the passive delivery of nutrients through food and water. That is, when an individual is consuming a fortified food or drinking fluoridated water, the sole and primary purpose of that act of consumption is not necessarily to replenish the nutrient which the food or water is fortified with. The passive consumption of nutrients is in fact the hallmark of these interventions as they do not require any lifestyle change to gain the benefits of consuming the nutrient. This, it can be argued, constitutes an infringement of individuals’ autonomy and their interest in self-determination.
Ethical Frameworks
Despite the different delivery mechanisms and ailments treated by food fortification and water fluoridation, the similarities regarding intent, passive delivery, and the lack of an informed consent procedure render the two types of public health interventions ethically similar. The corresponding ethical dilemmas and questions regarding intent, passive delivery and the lack of an informed consent necessitate a thorough analysis of the ethical frameworks used to evaluate food fortification and water fluoridation.
Two examples of ethical frameworks used to evaluate public health interventions are the justificatory approach of James Childress and the stewardship model of the Nuffield Council on Bioethics. The justificatory approach consists of the following tenets: effectiveness, proportionality, necessity, least infringement and public justification [25]. The stewardship model considers these principles: reduce the risk of ill health, address the health of children, reduce health inequalities, not intervene without the consent of those affected, minimize the interventions that affect important areas of personal life and not coerce ordinary adults to lead healthy lives [26]. Mark Lawrence applies the justificatory approach for all his food fortification case studies as does Niyi Awofeso to water fluoridation [27, 28]. Jiang et al. and the Nuffield Council of Bioethics use the stewardship model in their evaluation of water fluoridation in New Zealand and the United Kingdom respectively [22, 29].
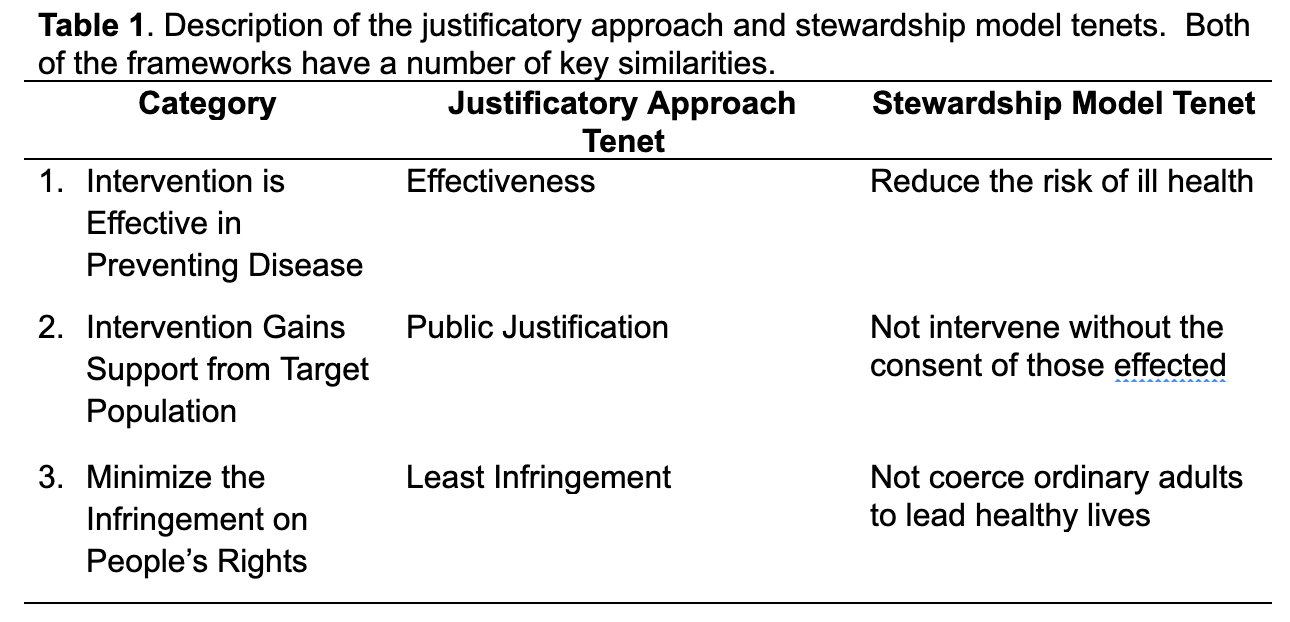
Table 1 concisely displays how the tenets of both the justificatory approach and stewardship models overlap and agree. Nonetheless, differences between the frameworks should not be overlooked, particularly the fact that the stewardship model places a particular interest in the health of children and focuses on health inequalities in the population. Despite these differences, ethical analyses of food fortification and water fluoridation shows that similar, even identical frameworks lead to opposite ethical judgements. A distinct example of this is the consideration of coercion by Jiang et al. and Lawrence. Jiang et al. argue that water fluoridation is inherently not coercive as it does not require any lifestyle change [29], while Lawrence claims that mandatory folic acid fortification of flour is coercive as it indiscriminately raises folate levels for everyone [27]. This differing definition of the term “coercion”, shows that even within ethical frameworks, having a provision to minimize coercion is not sufficient without an agreed-upon definition of the term. The coercion argument against public water fluoridation is further supported by the availability and near universal, non-coercive use of fluoridated toothpaste. In addition, evidence within the past decade has shown that low chronic daily intake of fluoride is a health risk associated with dental fluorosis and unhealthy fluoride accumulation levels within the body [30].
The passive consumption and the implied deception associated with water fluoridation and food fortification is overlooked by both the justificatory approach and stewardship model. Where this definition of deception directly relates to the ethics of food fortification and water fluoridation is in the fact that consumers are not necessarily fully aware of the entirety of their foods’ composition. While the FDA in the United States does have labeling requirements for fortified foods and salt [31] and also recommends that individuals in a community should know about fluoride levels in their water [32], this does not necessarily override the claim of deception being present in these interventions. With fortified foods, the final consumer of the food is not necessarily the purchaser of the ingredients which the food is made with (as in the case of eating food prepared by someone else). In addition, the knowledge of additional nutrients in the ingredients is further dispersed from the final consumer, perpetuating the deception of fortified foods.
Douglas Cross and Robert Carton take a more linear view on fluoridation [33]. Their argument starts with the fact that the Nuremberg Code (and all successive ethics codes derived from it) prescribes: “research and routine medical procedures must be done with the voluntary cooperation of the subjects, who must be fully informed of the risks and benefits of the medical procedures in which they are involved”. From this, Cross and Carton establish that fluoride is a medicine according to definitions from European and American pharmaceutical codes (generally defining medical substances as products used for treating or preventing disease in humans or animals) and point out that fluoride is not governed by the Nuremberg Code, rendering it unethical. This argument does tap into the problem of deception in water fluoridation, as passive consumption prevents the consumer from being “fully informed of the [procedure’s] risks and benefits”. Furthermore, this argument is easily transferrable to food fortification as adding nutrients to food does exhibit the qualities of a medicinal substance: nutrients such as folate and iodine have a preventive role in human illness (folate and iodine prevent neural tube defects and goiter respectively), and also do not fully adhere to the principle of informed consent.
Conclusions
Food fortification and water fluoridation interventions are very similar in that they do not involve a direct clinician-patient interaction and rely on the “patient’s” lack of knowledge and passive consumption of the target nutrient. The justificatory approach and the stewardship models both support from an ethical standpoint the processes of water fluoridation and food fortification. Nevertheless, both ethical frameworks display shortfalls after careful analysis and considerations of other opinions critical of food fortification and water fluoridation. In light of recent public discourse surrounding the delivery of therapeutics to the public through passive consumption, it is important that we revisit and continue to analyze the ethical frameworks that govern the already widely accepted interventions of food fortification and water fluoridation.
References
1. Sirtori CR (2014) The pharmacology of statins. Pharmacol. Res. 88:3–11
2. Bishai D, Nalubola R (2002) The History of Food Fortification in the United States: Its Relevance for Current Fortification Efforts in Developing Countries. Econ Dev Cult Change 51:37–53. https://doi.org/10.1086/345361
3. Krishnan A V., Trump DL, Johnson CS, Feldman D (2010) The role of vitamin D in cancer prevention and treatment. Endocrinol. Metab. Clin. North Am. 39:401–418
4. Dwyer JT, Wiemer KL, Dary O, et al (2015) Fortification and health: challenges and opportunities. Adv Nutr 6:124–31
5. Ong HT (2006) Evidence-Based Prescribing of Statins: A Developing World Perspective. PLoS Med 3:e50. https://doi.org/10.1371/journal.pmed.0030050
6. Ridker PM, Danielson E, Fonseca FAH, et al (2008) Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 359:2195–2207. https://doi.org/10.1056/NEJMoa0807646
7. Savules J (2008) Fluoride and the Future: Population Level Cognitive Enhancement | Practical Ethics. In: Ethics News Oxford Univ. . http://blog.practicalethics.ox.ac.uk/2008/02/fluoride-and-the-future-population-level-cognitive-enhancement/. Accessed 9 Sep 2019
8. Allen L, De Benoist B, Dary O, Hurrell R (2006) Guidelines on food fortification with micronutrients. Geneva, Switzerland
9. Crider KS, Bailey LB, Berry RJ (2011) Folic Acid Food Fortification—Its History, Effect, Concerns, and Future Directions. Nutrients 3:370. https://doi.org/10.3390/NU3030370
10. Leung AM, Braverman LE, Pearce EN (2012) History of U.S. iodine fortification and supplementation. Nutrients 4:1740–6. https://doi.org/10.3390/nu4111740
11. Calvo MS, Whiting SJ, Barton CN (2004) Vitamin D fortification in the United States and Canada: current status and data needs. Am J Clin Nutr 80:1710S–1716S. https://doi.org/10.1093/ajcn/80.6.1710S
12. Centers for Disease Control and Prevention (2014) Water Fluoridation Additives Fact Sheet. http://fluoridealert.org/content/water-fluoridation-additives-fact-sheet/. Accessed 26 Jul 2019
13. Canadian Agency for Drugs and Technologies in, Health (CADTH) (2019) Community Water Fluoridation Programs: A Health Technology Assessment — Environmental Assessment. Ottawa, Canada
14. American Dental Association (2018) Fluoridation Facts
15. Mullen J (2005) History of Water Fluoridation. Br Dent J 199:1–4. https://doi.org/10.1038/sj.bdj.4812863
16. Kanduti D, Sterbenk P, Artnik B (2016) Fluoride: A Review of use and effects on health. Mater Sociomed 28:133–7. https://doi.org/10.5455/msm.2016.28.133-137
17. Koulourides T (1990) Summary of Session II: Fluoride and the Caries Process. J Dent Res 69:558–558. https://doi.org/10.1177/00220345900690S111
18. Featherstone JDB (1999) Prevention and reversal of dental caries: role of low level fluoride. Community Dent Oral Epidemiol 27:31–40. https://doi.org/10.1111/j.1600-0528.1999.tb01989.x
19. Truman BI, Gooch BF, Sulemana I, et al (2002) Reviews of evidence on interventions to prevent dental caries, oral and pharyngeal cancers, and sports-related craniofacial injuries. Am J Prev Med 23:21–54
20. Griffin SO, Regnier E, Griffin PM, Huntley V (2007) Effectiveness of Fluoride in Preventing Caries in Adults. J Dent Res 86:410–415. https://doi.org/10.1177/154405910708600504
21. Howard Pollick (2015) Current issues in the science of community water fluoridation. https://www.ada.org/~/media/ADA/Public Programs/Files/Pollick.pdf?la=en. Accessed 3 Sep 2019
22. Nuffield Council on Bioethics (2007) Public health: ethical issues. London, UK
23. Food and Drug Administration (FDA) (2016) Raw Dough’s a Raw Deal and Could Make You Sick. In: FDA. https://www.fda.gov/consumers/consumer-updates/raw-doughs-raw-deal-and-could-make-you-sick. Accessed 2 Sep 2019
24. Ginter E, Kajaba I, Sauša M (2012) [Addition of statins into the public water supply? Risks of side effects and low cholesterol levels]. Cas Lek Cesk 151:243–7
25. Childress JF, Faden RR, Gaare RD, et al (2002) Public Health Ethics: Mapping the Terrain. J Law, Med Ethics 30:170–178. https://doi.org/10.1111/j.1748-720X.2002.tb00384.x
26. Nuffield Council on Bioethics (2007) Public health: ethical issues
27. Lawrence M (Mark A (2013) Food fortification : the evidence, ethics, and politics of adding nutrients to food. Oxford University Press
28. Peckham S, Awofeso N (2014) Water fluoridation: a critical review of the physiological effects of ingested fluoride as a public health intervention. ScientificWorldJournal 2014:293019. https://doi.org/10.1155/2014/293019
29. Jiang Y, Foster Page LA, McMillan J, et al (2014) Is New Zealand water fluoridation justified? N Z Med J 127:80–6
30. National Research Council (2006) Fluoride in Drinking Water: A Scientific Review of EPA’s Standards. The National Academies Press, Washington, DC
31. Center for Food Safety and Applied Nutrition (2015) Contains Nonbinding Recommendations 1 Questions and Answers on FDA’s Fortification Policy Guidance for Industry
32. U.S. Food & Drug Administration Code of Federal Regulations - Title 21 - Food and Drugs | FDA. https://www.fda.gov/medical-devices/medical-device-databases/code-federal-regulations-title-21-food-and-drugs. Accessed 26 Jul 2019
33. Cross DW, Carton RJ (2003) Fluoridation: A Violation of Medical Ethics and Human Rights. Int J Occup Environ Health 9:24–29. https://doi.org/10.1179/107735203800328830

