A New Frontier in the Fight Against Cancer (That Is, for Those Who Can Afford It) The Approval and Cost of CAR T-Cell Therapies
Main Article Content
Abstract
The Food and Drug Administration (FDA) made history this fall with its approval of Novartis’s Kymirah and Gilead’s Yescarta—the first gene therapies to ever be approved in the United States. [1,2] Both treatments belong to a new class of cancer therapeutics called CAR T-cell treatments, which use patients’ own immune cells to fight cancer.[1,2] These approvals may therefore mark the dawn of a new day for both gene therapy and the treatment of cancer.
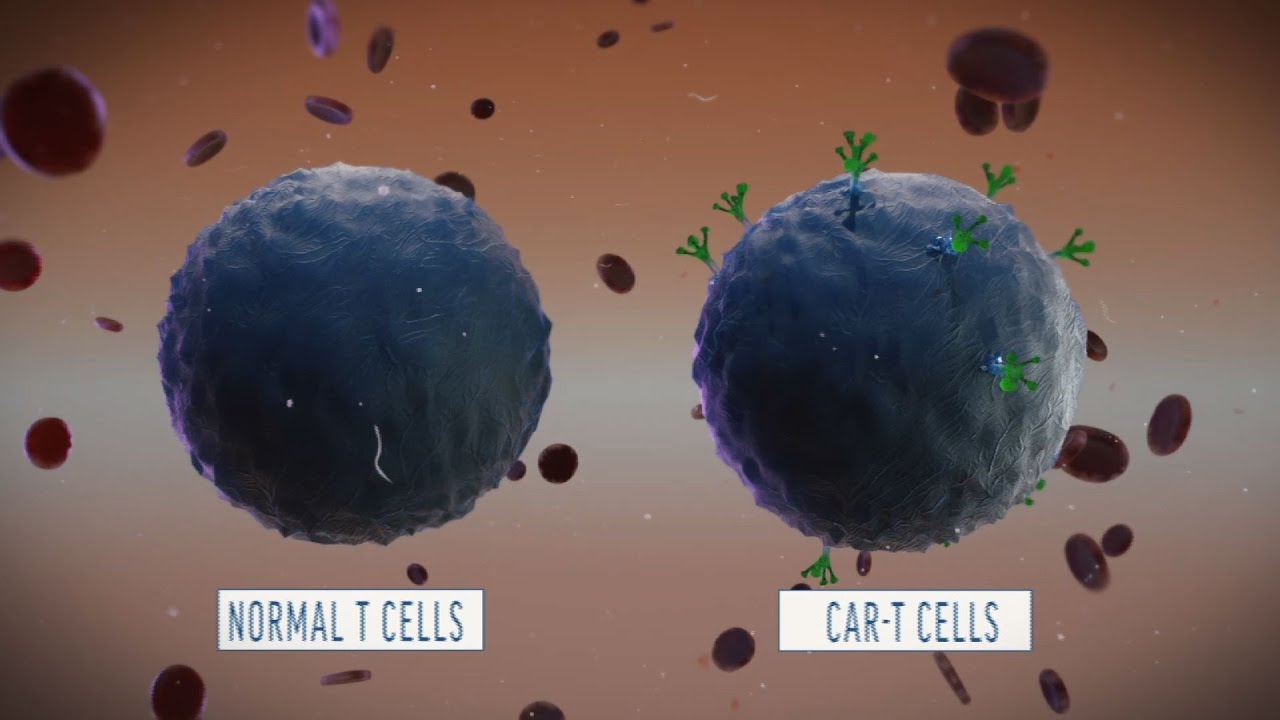
The manufacture of CAR T-cell treatments begins with the collection of T-cells, a type of white bloods cells, from a patient.[3] These cells are then genetically modified using a viral vector to express a protein known as chimeric antigen receptor (i.e., CAR). Once injected back into the patient, CAR causes the T-cells to seek and destroy cancer cells, combating the disease with seemingly unprecedented efficiency.[3]
Kymirah, for example, caused 83% of 63 juvenile clinical trial subjects with a certain type of leukemia to go into remission within three months of receiving treatment.[1] Yescarta showed similar promise in clinical trials by sending 51% of the 100 adult subjects with B-cell lymphoma into complete remission.[2] Because these treatments must only be administered once, many see these drugs not as cancer treatments, but as cancer cures—a paradigmatic shift in the fight against cancer.
Both drugs, however, are not without their serious side effects. For instance, both treatments can induce cytokine release syndrome (CRS), an immune system response to the presence of CAR T-cells that can cause high fever, flu-like symptoms, and potentially life-threatening neurological events.[1,2] Other serious side effects include: infection, hypotension, kidney damage, and hypoxia.[1.2] Given these significant risks, the FDA approved both Kymirah and Yescarta pursuant to a risk evaluation mitigation strategy (REMS), which, among other things, requires hospitals and clinics to obtain special certification in order to dispense these drugs.[1.2] To become certified, personnel must undergo training to recognize and treat CRS and hospitals and clinics must have the appropriate medications to treat CRS on hand.[1,2] Furthermore, due to their associated risks, both treatments are approved only as a drug of last resort (i.e., after all other treatments have failed).[1,2] By taking steps to reduce the risks associated with these uniquely effective treatments, the FDA seems to have appropriately accounted for the bioethical principles of nonmaleficence and beneficence. However, given their exorbitant costs, these drugs do pose some concerns for the bioethical principle of justice.
Kymirah is currently sold by Novartis for $457,000, while Yescarta is available for the slightly less eye-popping price of $373,000.[4,5] Moreover, because these drugs will be available only at certified institutions, many will have to incur travel costs to gain access to these treatments. The hefty costs associated with these drugs have further stoked the uproar against rising drug prices.[4] Specifically, some to fear that, given the efficacy of these drugs, cancer will someday be a disease reserved only for the poor.[4] Such an outcome would for obvious reasons exacerbate the already problematic opportunity gaps that plague our country.
Manufacturers of these drugs, however, attempt to justify high prices by pointing to the fact that these drugs effectively constitute cancer cures.[4,5] Consequently, patients must only pay once for these drugs instead multiple times over the course of several years as with traditional treatments. This justification, however, is made slightly less persuasive by the fact that these drugs are approved only as a last line of defense. As such, patients must endure costly treatment regimens before they’re asked to shell out almost half a million dollars for CAR T-cell therapies.
Novartis, however, has said that it will only charge patients who respond to Kymirah within a month of receiving treatment; the company is currently working with the Centers for Medicare and Medicaid Services to design a payment plan to that effect.[6] Novartis has also stated that it “will offer an access program in the U.S. for eligible uninsured and underinsured patients” while “payers are developing their payment policies” for the drug.[6] Gilead has yet to make similar announcements regarding Yescarta.
Debates regarding the costs of gene therapies are likely to heat up as more treatments of this kind are approved. Other drug companies also developing gene therapies have already indicated that their products, if approved, will carry similarly high price tags.[4] These companies, however, likewise justify the high costs. They claim that the prices are warranted given that these therapies: 1) can offer a cure for otherwise intractable conditions and 2) often target rare conditions and must therefore be priced highly in order to draw a profit.[4] It is possible, however, that, as with any technology, the price of these treatments will drop over time. That may be particularly true if CRISPR-Cas9, the most cost-effective gene-editing technique discovered to-date, eventually replaces viral vectors as the primary means for creating gene therapies. Also, insurers are discussing ways to devise alternative payment models for gene therapies such as paying for a treatment over time, the establishment of insurer risk pools, and the potential financing of one time payments.[6]
How all this will play out remains to be seen, but pharmaceutical companies and policy-makers must take the appropriate steps to ensure that these promising new therapies don’t ultimately lead to the ghettoization of cancer and other genetic diseases.
Works Cited
1. FDA News Release, FDA Approval Brings First Gene Therapy to the United States, (Aug. 30, 2017), https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm574058.htm.
2. FDA News Release, FDA Approves CAR-T Cell Therapy to Treat Adults with Certain Types of Large B-Cell Lymphoma, (Oct. 18, 2017), https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm581216.htm.
3. National Cancer Institute, CAR T Cells: Engineering Patient’s Immune Cells to Treat Their Cancers, (Aug. 31, 2017), https://www.cancer.gov/about-cancer/treatment/research/car-t-cells.
4. Gina Kolata, New Gene-Therapy Treatments Will Carry Whopping Price Tags, New York Times (Sept. 11, 2017), https://www.nytimes.com/2017/09/11/health/cost-gene-therapy-drugs.html.
5. Toni Clark and Bill Berkot, FDA Approves Gilead Cancer Gene Therapy; Price Set at $375,000, Reuters (Oct. 18, 2017), https://www.reuters.com/article/us-gilead-sciences-fda/fda-approves-gilead-cancer-gene-therapy-price-set-at-373000-idUSKBN1CN35H.
6. Arlene Weintrab, How to Cover Novartis’ $475K CAR-T Drug Kymirah? A’New Payment Model’ is the Only Way, Express Scripts Says, (Sept. 22, 2017), https://www.fiercepharma.com/financials/car-t-and-other-gene-therapies-need-new-payment-model-says-express-scripts.