Implementing Personalized Genetic Medicine Interprofessional and Patient Perspectives on Connecting Medical Research with Clinical Care
Main Article Content
Abstract
Photo by AbsolutVision on Unsplash
ABSTRACT
This qualitative interview study explores the implementation of personalized genetic medicine (PGM) for prostate cancer in a major university hospital in Finland. We interviewed both staff and patients. University hospital staff (n = 12) were interviewed concerning their views about the promises and challenges of the new medicine. The six patient research subjects taking part in a prostate cancer PGM study were interviewed about their experiences. The two sets of interviews were analyzed separately in a qualitative thematic analysis rooted in the theory of social constructionism. The staff interviews brought out the following themes: entanglement of research and care, professionality, context, scientific breakthrough, technocracy, and emotional engagement. In the patient interviews, the following themes were discovered: personal narrative, autonomy, community, and relationships with staff. These results demonstrate that staff and patients both experience entanglement of research and care but they speak about the implementation process using disparate language. Based on the research, we conclude that research design as well as legislative processes would benefit from inclusion of broad perspectives as expressed by those engaged in the experience of research as patients or as practitioners.
INTRODUCTION
Contemporary advances in biomedical sciences related to genomic sequencing and molecular characterization are changing the landscape of cancer treatment and research at a fast pace.[1] Even though central questions regarding research ethics (such as uncertainties about ensuring informed consent)[2] remain, cancer patients, continue to enroll in personalized medicine research studies. Implementation of PM would include “a need for restructuring the healthcare system—detachment of healthcare professionals from the so-called organ-based specialties.”[3] This study explores the experiences of the staff and patients involved in clinical research in personalized medicine. To be more precise, in this qualitative social scientific study, we explore the narratives of the stakeholders that are involved in a study of a precision medicine (PM) for genetic prostate cancer taking place at a major university hospital in Finland to learn about their experiences and viewpoints.
Personalized medicine broadly refers to the tailoring of care to patients’ individual attributes, typically in relation to their genomic, genetic, and molecular profile.[4] Compared to traditional evidence-based medicine, PM represents a shift toward viewing each disease and patient as biologically unique.[5] Proponents of PM advocate moving away from blockbuster drugs in favor of individualized, tailored treatment options that consider each patient’s pharmacogenomics profile.[6] However, this shift raises several issues for consideration, such as how to ethically test drugs in very small patient groups, what conclusions can be appropriately drawn and generalized, and how to establish accessible and equitable practices for implementation in the future.[7] The interviewees noted blurring of the line between clinical therapeutic use and research purposes. In this paper, we use the term patient or research patient to mean the research subjects that are patients.
Increased patient empowerment is achieved when individuals gain control over planning their healthcare services.[8] President Barrack Obama’s 2015 Precision Medicine Initiative promoted these concepts, advocating for “patient-powered research,” in which “participants will be involved in the design of the initiative and will have the opportunity to contribute to diverse sources of data.”[9]
This interview-based study focuses on the implementation of personalized genetic medicine (PGM) and is contextually connected to a concurrent biomedical study aimed at the genetic profiling of patient prostate cancer cells to report clinically meaningful results to treating clinicians. We interviewed relevant stakeholders, including staff and research patients, to assess how they view the potential promises and risks of personalized genetic medicine, and whether they see the high expectations of PGM as challenging the traditional boundaries between research and care activities in the lab and clinic. We used the responses provided during the interview process to understand how those involved in prostate cancer PGM research make sense of this new practice.
l. DATA AND METHOD
a. Semi-structured Interviews
The thematic interviews followed a loosely predesigned form, still giving relative freedom for the interviewees to explore additional topics. We selected participants for this study from current university and hospital staff to participate in an interview with questions involving the following themes: how participants view overall differences between research and care, participant beliefs about whether PGM blurs these boundaries, participant expectations for PGM, and ethical challenges envisioned in the implementation of PGM.
We asked patient research subjects about their motivations for participating in the ongoing PGM study, the differences they see between their clinical care and research participation, the process of giving consent, the sources they used for gathering information related to the study, and the potential hopes and fears they had for the genetic analysis of their prostate cancer cells.
b. Data Collection
A total of 19 audio-recorded interviews varying between 45 and 75 minutes in length were collected for this study. Interviewed staff members consisted of both university and hospital personnel from the following backgrounds: one bioinformatician, biomedical researchers (n = 4), physician-researchers (n = 3), research nurses (n = 3) and IRB members (n = 2). Additionally, six patient research subjects were interviewed.
We interviewed university and hospital staff between February 2016 and May 2017. The collection of staff interviewees was based on snowball sampling, a method in which the respondents are themselves used to recruit further respondents from their social networks. Snowball sampling was used because no clear sample frame exists for the study.[10] The patient research subject interviewees were contacted based on their enrollment in the background PGM study during the year 2017. The research subjects for that clinical study had been chosen based on a profile of a high risk for recurrence of prostate cancer.
c. Theory and Analysis
While there is no single description of social constructionism, its fundamental claim is that knowledge is not objective in its nature, but rather constantly shaped and sustained by ongoing social processes. What passes as knowledge in a given culture is then, “not a product of objective observation of the world, but of the social processes and interactions in which people are constantly engaged with each other.”[11]
What emerges from our study is a refined understanding of the social reality of implementing PGM as perceived by those personally involved in it, which we believe is a fruitful and enlightening contribution to the growing literature on personalized medicine.
The interviews were analyzed with the qualitative method of thematic analysis, which is “a method for identifying, analyzing, and reporting patterns (themes) within data.”[12] The method is used in this study as anchored in the social constructionist epistemology. Following Braun and Clarke, we carried out the analysis process in six phases. The phases were 1) familiarizing ourselves with the data (in which the manual transcription process was a significant element), 2) generating initial codes in the data by color coding the text, 3) searching for initial themes among the codes, 4) reviewing the themes by iterative reading of the data, 5) defining and naming the themes discovered, and 6) writing the final report.[13]
d. Ethical Considerations
Prior to conducting interviews, participants were informed of the study and given the opportunity to refuse or cancel participation at any point. The interview data collected during this study have been used only for the purposes of this study. Before proceeding to the interviews, the research plan was also reviewed and accepted by the local ethics committee for humanities and social sciences.[14] Participants have been anonymized to protect their identities, as implementing PGM for prostate cancer in Finland is limited to a fairly marginal group of professionals and patients.
ll. RESULTS
The findings of this study are presented in two parts: themes discovered in staff interviews, and themes discovered in the research patient interviews. The transcripts presented below have been translated from Finnish into English and have been categorized by their identified themes.
lll. STAFF INTERVIEWS
a. Entanglement of Scientific Research and Clinical Care
Our first discovery was that most of the interviewed professionals experienced an entanglement between research and care practices. However, those with IRB backgrounds expressed very clear boundaries between the two practices.
The following interview excerpt demonstrates the typical entanglement of research and care that we found in our interviews. An interviewed physician perceived research as the best kind of care, giving “the patient many extra benefits.”
A: Research is care of the patient, it just happens within a research protocol in which some new form of treatment is compared to the old treatment. (…)
Q: So what do you think, is there a boundary between research and care or not?
A: Yeah of course in that way that you go through this same procedure we just did [with this interview study], the patient is informed by the study and then gives his consent if he wants to participate, and usually he does, because of course it gives the patient many extra benefits, the monitoring is much closer, and you get the same doctor and nurse, usually quite long relationships with the same staff.
- Physician-researcher
The following interviewee illustrates an underlying belief that receiving care in studies that are funded by pharmaceutical companies is beneficial for society, as it relieves government as a payor.
Patients should be in research studies because it is much cheaper for society, so that there is not so much municipal billing… Nobody can really count how much is saved, but of course when the medicine comes from the study there are a lot of savings made, maybe…
- Research nurse
Interestingly, several of the scientists interviewed constructed the mission of their work in the words of curing patients (in the long run), and not as one might assume, as generating knowledge that might contribute to curing patients in the long run.
For me it’s very important that there is a clear goal for why this research is done… (…) I myself experience a strong sense of direction, even if it is in the distant future… (…) The goal is that cancer could be, wiped out, and people cured, that’s how I see it.
- Biomedical researcher
However, another participant constructed the two practices as fundamentally separate:
In clinical care with patients, of course we are concentrating on that patient’s issues, whereas when we are doing research we are looking at, larger entities and phenomena. I think doing both gives great variety to my work.
- Physician-researcher
b. Professionality: Expertise, Ethics, Trust, and the Tolerance of Uncertainty
Professionality was distinguished by those interviewed based on three central dimensions: expertise, following shared ethical standards, and being able to adopt an attitude of tolerance toward uncertainty in the practice.
First, expertise, referring to knowledge and skill, was constructed as the center of professionality. However, this quality was defined quite loosely; it was surprisingly hard to describe exactly who is a professional and who is not. The next example shows how a medical professional believes his knowledge and skill can even be associated with someone wearing a clinical uniform, the uniform fostering the basis for the patient’s trust.
I don’t think it matters to the patient who asks for the consent, except that the patient probably doesn’t want to talk to someone in a civil outfit, in a pleated skirt or a dress shirt, no, the patient trusts a professional, a doctor or a nurse who can explain… So I don’t think it matters who it is, as long as it’s someone the patient can trust.
- Research nurse
One participant asserted that a deeper relationship contributes to trust in patient interactions during the research, distinguished from routine clinical interaction.
I form a very deep relationship, with the research patients since they have such an intensive, I mean they have a straight connection to me in every way, even though the doctor is the most important, the nurse still comes before that, like if they wonder about something in the evening they call the nurse, we have a phone 24/7 that the patients can call. (…) I think this is the best personal care there is, very very good personal care, and in most cases, everybody trusts each other, they trust that with me they are in safe hands.
- Research nurse
The capacity to endure uncertainty presents another key element in the theme of professionalism.
Clinical work is constant tolerance of uncertainty, you just have to go by the probabilities and, accept that you can never be 100 percent sure, but maybe researchers are like, they have to look for the accurate, precise answer to everything, and so I think that could maybe create some problems for the collaborations…
- Physician-researcher
c. Context: Culture, Community, and the Efficiency Imperative
Contextual talk refers to the institutional and cultural environment surrounding research and care. Most commonly, interviewees mention Finnish culture by praising “Finnish patients” as more agreeable to research than patients from other countries. This notion was expressed across the wide range of professionals interviewed.
Of course, we have always said that they can withdraw from the study if they want, but here, these Finnish patients are so kind, and they trust the physician so much, the physician’s authority is so great… (…) We have, such kind patients that they always come [to the research tests], they follow the protocol very strictly.
- Research nurse
Sometimes we make quite invasive [research] operations, and while we know that Finnish patients will participate, we have sat down [with colleagues] to think about it, that… they are giving their consent but are we doing harm…
- Biomedical researcher
Another contextual factor expressed by interviewed professionals was the benefit of belonging to a work community. The community was portrayed as not only providing knowledge and team effort, but also emotional support for the staff.
Now that I finally have this office here, the other research nurses are close by, so I can share if I have something on my mind, like stress or something.
- Research nurse
A concern regarding imposed demands on clinical efficiency was identified as part of the contextual theme. In these examples, efficiency serves as the first principle to which everything else is to conform, such as ethical recruiting of research patients.
Time is, right now, a great problem, and because of the lack of it, an individual can vanish into the mass, since we just don’t have enough time for the patients individually.
- Research nurse[15]
What efficiency does is that the patients are in the hospital for a very short time, they go straight to the operating room, so they are there before that for maximum 2 hours if we’re talking about surgery patients, and this makes the researcher’s work [considering ethical research recruitment] so much more complicated. (…) And it depends on the funding whether the researcher has enough time to spend on properly informing the research subject.
- IRB secretary
d. PGM as a Scientific Breakthrough: Progress, Ambition, and the Critique of the Status Quo
Interestingly, even though our informants did not separate clinical care from clinical research clearly, we found a theme of science distinct from the everyday clinical practices. This theme was not defined in terms of the everyday research environment, but instead, as a bird’s eye view: as being able to adopt a broader scale of thinking in a way that was something different from or more than the everyday realities.
Interestingly, in the theme of science, we found a struggle about the future of PGM and whether to believe PGM is a promising scientific breakthrough instead of science hype. The next samples show an enthusiastic as well as a more skeptical point of view toward PGM.
Things can only go to a better direction here since [because of PGM] we will treat people better and better, even though it is obvious that it is not going to cheap, that’s the first question, but I think that in the long term there will be less expenses at a public health level when there you take into account the prevention of diseases and health coaching and things like that.
- Bioinformatician
The genetic research eats up a lot of resources and still, from a clinician’s point of view, the outcome is quite small, like for example we still don’t have very good genetic tests that could predict, in a clear way, that a patient has specifically this kind of cancer and it’s going to proceed this way so let’s treat it in this way, like still we have pretty much the same, Gleason points and PSA tests that we’ve had for the past 50 years, or longer, even though billions have been spent on genetic research.
- Physician-researcher
e. PGM as a Technocratic Challenge: Bureaucracy and the Law
Participants identified additional themes involving clinical research in PGM that concern bureaucracy and paperwork, disclosure, and consent requirements taking shape in legislative forums, referred to here collectively as “technocratic”. This theme reflects new legislation, policy, and procedures required for medical research. Professionals expressed concern that the current legislation and structures may be standing in the way of valuable scientific improvements.
We need new ways to validate the drugs, and the question is, is this ethically on solid ground, since there are reasons, historical reasons for why the process of developing drugs is so complicated.
- Biomedical researcher
Technocratic practices, like the need for documenting informed consent, were also criticized for being too complicated. In the following sample, a research nurse expressed frustration with having to ask patients recovering from surgery to fill out consent forms.
Like if we have a bladder cancer patient who has just had surgery in the ward, I have to run in there to ask for a pre-pre-permission, to ask whether they can use a part of his bladder, which is already on the pathologist’s table at that point, for some research… It’s a miracle they even have energy to write when they [the patient] are on the IVs and cannulas and everything, and there I have to say to them, please write down the date and print your name here…
- Research nurse
The IRB interviewees also presented critical views about the research bureaucracy.
We do so much education because the researchers are in such a jungle, I don’t want to blame them, the jungle is absolutely absurd, the clinical researcher has to consider all the legislations, of course they have to have the law, the clauses and the ethical reviews in check, but it takes such a huge amount of time for them to figure it all out.
- IRB Secretary
f. Research as Emotional Engagement and Empathy
Sentiment and empathy play an important role for professionals in their work and attitude toward research, evidencing emotional engagement.
Over the years I have developed a sort of, doctor’s conscience, I can’t do things if I know that I’m going to do them badly, or wrong, that’s when I won’t get a peace of mind for myself, so I better do things best I can because otherwise it bothers me so much… Of course it is a subjective point of view but, I can’t, can’t do things badly or wrong to a patient.
- Physician-researcher
One researcher expressed the need to protect herself from feeling emotional toward patients.
I see myself as quite a sensitive person, and it has been my conscious choice that, I like that the research patients are anonymous to me, so that the sample (…) is not personified.
- Biomedical researcher
A second researcher suppressed emotions surrounding the research because of the gravity of the situation to patients.
I have mixed emotions, because for research it is a good thing to get test samples from patients who have metastases in their lymph nodes, not only patients who just have cancer in the prostate. (…) I really feel bad that I can’t be happy that now there is a person somewhere who has had these metastases.
- Biomedical researcher
lV. RESEARCH PATIENT INTERVIEWS
a. Personal Narrative: Life Story, Worldview, and Character
Personal narratives include reports of personal life situations, illness histories, worldviews, and descriptions of character. We asked patients about their motivations to participate in the PGM study. Responses included patients’ complete past medical histories and key moments that led to their diagnosis and subsequent participation in this study. The next example shows that the illness narrative represented to us could even go as far back as the interviewee’s childhood.
I haven’t been ill very much, but in 1955, I was born in 1950, so 1955 I got hit by a car, and my right shin was fractured, they fixed it in the local hospital, the surgeon was called [name], as I asked my mother about it later, so this doctor [name] had said to my mother that he fixed the leg and he fixed it well.
- Research patient (Interview 1)
Additionally, personal narratives reflected the collective strength derived from family.
It is a really personal thing… the way you deal with something like this… We dealt with things the way that, my son said well, you have made it through worse, he just said you have made it through worse, it is, it really is true that we have always survived, as life has been really long and troublesome, or if not troublesome at least really tough.
- Research patient (Interview 6)
The personal narratives also described worldviews, the below suggesting a lack of desire to have psychosocial support.
Q: Did you get any [psychosocial] support when you first heard the diagnosis?
A: It doesn’t really help anything, if you are doomed you are doomed… But for me, it is God up there who takes care.
- Research patient (Interview 1)
b. Autonomy: Context and Knowledge as the Foundation for Decision Making
Talk about making decisions, knowledge, and gathering information were categorized as expressions of autonomy and also included talk about knowledge and searching for information as part of the theme. People varied in how much they value information as a key element of decision making. The next two data samples demonstrate the wide range between the interviewees, one seeking information on the internet, the other preferring not to read the provided information or seek other sources.
Q: Was your decision based on what the doctor told you or did you search for knowledge yourself, for example on the internet?
A: Yes, [the] internet is where you look for knowledge these days, the doctor didn’t really give an opinion… I think reading text and thinking about what you have read is important, things you just hear in a briefing really get lost if you don’t have enough background information, so you can’t really have an opinion and think about it at that point, but of course [the] internet is a little like that too, so you have to be mindful about what you are reading… there are, lots of things you shouldn’t believe in…But I think all sort of medical publications and such, that’s where the information came from.
- Research patient (Interview 4)
Q: Did you find out about the research topic independently online or…?
A: No… Not at all, not at all (with laughter), I also got all those papers [from the staff] too and I didn’t read a single one of them… I decided I won’t read any of it, better if I don’t know, I will go completely ignorant, because I think information increases the pain (laughter).
- Research patient (Interview 2)
As in the staff interviews, the patients had difficulty keeping the research and the clinical care separate during the interviews. We found the topics were entangled especially because they both took place in the same surroundings, usually organized by the same people. In the next example, the research participant expressed feeling pressure to participate because he was already a patient of the recruiting doctor.
This research came up at the point which, [name of doctor] was explaining, before the surgery how the surgery will be done, and so, he introduced the study, asking if I could participate and so, I couldn’t really say no, I couldn’t really say that you just do the surgery but I won’t participate… (Laughter) Because I think that if someone can benefit [from my participation in the study], then of course it’s a good thing if someone gets help.
- Research patient (Interview 1)
Participant decisions are made within an already existing and meaningful social network in the hospital environment, with embedded cultural norms in place, such as reciprocity. These findings show how differently people make their decisions and that autonomy appears to be a socially embedded, nuanced, and ambiguous concept, varying from person to person.
c. Community: Receiving Support and Mirroring Experiences
Being part of a community and sharing experiences was a central theme in our patient interviews.
I play table tennis, and the playing community (…) is good for psychological wellbeing, I have been able to talk openly, even at that point when the cancer was diagnosed and so, it makes things much easier when you don’t have to live in secrecy.
- Research patient (Interview 4)
I went through them [the treatment options] with my wife very thoroughly, and eventually, we made the decision together.
- Research patient (Interview 5)
However, not everybody accessed support from others:
I didn’t really have any social network for support, I just talked with the staff that this is the way things are, what else is there to say about it.
- Research patient (Interview 2)
Social communities with members with similar experiences influenced participants’ decisions.
Well it wasn’t clear at first, but I thought about it and little by little I decided on the surgery, as it had gone so well for my brother one year earlier, (…) we did talk about the options with the doctor and I was just repeating that I want the surgery, so I made the decision myself, because I knew what the options were.
- Research patient (Interview 1)
The quotes demonstrate how a social network serves both as a structure for support and therapeutic decision making.
d. Relationships With Staff: Alliance and Distance
We divided patient relationships with staff as those of either alliance or distance.
Relationships of alliance that cultivated respect, trust, and a feeling of being taken care of resulted in patient satisfaction and gratitude.
So the results were discovered and the treatment options, and so we discussed what this and that surgery is, and so, it was very good in many ways, I got all the information I could think of… and, well, the whole process just radiated expertise, and that really awakened trust in me.
Research patient (Interview 3)
In some cases, the alliance was not necessarily focused on any specific person but instead on the hospital as an institution.
Whenever I walk through the hospital doors, I let go of all my worries, because I have always thought that there is staff and I have nothing to worry about, I know that they take care of me.
- Research patient (Interview 2)
The biomedical researcher who also acted as our contact person with the PGM study had a key role in the recruiting process. She would often walk the research patients in the hospital to different locations of the tests.
She came there, you see and walked with me, it was totally different, it was sort of safe, to have someone to walk with you and we could talk. Otherwise I would have been walking alone, but when she was with me we could talk about different things and I kind of forgot about everything else. I think everyone here should have someone like that…
- Research patient (Interview 2)
While one could also assume that contacts with staff members in positions of authority would reflect social distance, we found that authority increased the trust and respect and provided a foundation for a staff-patient relationship. In the next sample, the authority of the professor fueled the willingness to participate in the PGM research.
Yeah I could ask whatever I wanted, and he explained, (…) of course it feels good to get the possibility to talk with the professor like that.
- Research patient (Interview 2)
Interviewees also reported relationships with distance, doubts of whether the staff can be trusted, and stories of not being heard, but much less than they described alliance.[16] It was also typical that an alliance was described and compared to another situation in the past in which the patient had not been satisfied. In the next quote, the interviewee talked about his doubts about whether the hospital could be trusted to provide all the necessary care.
Well it was kind of a shock, or if not a shock then at least I had to think about what I should do now… everything just unfolded from there, people say that we have a good system in Finland, but I was asking whether I will get all the scans, the MRI, computer scan or the bone scan, or that… because I thought, they will look at me and think that I am old…
- Research patient (Interview 6)
In the next sample, an interviewee described his experiences with staff that resulted in feelings that he was not getting the help he needed.
I think it would really be important that the staff understands the importance of staying in close contact with the patients, to get the patient through all that, and just to generally offer some help, because, with the way things are now I think it is kind of a lonely man’s fight.
- Research patient (Interview 5)
V. DISCUSSION
In this study, we explored the diversity of voices intertwined with the process of implementing personalized genetic medicine for prostate cancer in a university hospital environment in Finland.
We embarked on this research with a view that medical research and clinical care are fundamentally separate activities. However, from the outset we found that the data was telling us otherwise. Even though “therapeutic misconception” has been documented widely elsewhere,[17] we were surprised by the impossibility of patients keeping the two categories apart, and especially with professionals’ inability to keep them apart. At first, we were frustrated about what seemed like not getting the right answers, but we started to see that the way people mix the categories of research and care is natural in the social process in which the patient and the staff work toward treating the cancer. The two appear naturally entangled in the university hospital environment. Making these everyday constructions visible in the Finnish context is an important implication of this interview study.
Another question is whether the differences found between the viewpoints of the professionals and the research patients matter. Has the medical establishment, with its institutional policy, law, and scientific method, veered too far from patients’ lifeworld? Or are these differences good for the research and care community, reflecting the expertise of professionals and the roles of those seeking care?
We have formed the image below to demonstrate the different perspectives relevant to the stakeholders in the process of implementing personalized medicine. The image represents the main viewpoints as a triangle, suggesting that while there are different perspectives, they are part of the same whole.
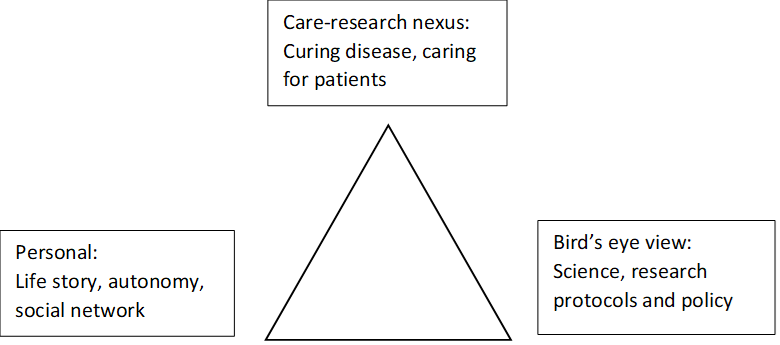
The three main perspectives entangled in the PGM implementation process could be used as an analytical tool for people designing research and healthcare policy. By including more perspectives in the dialogue, and propelling the patient voice that is often silent, the triangle would contribute to the development of policy and research studies. It is important to avoid framing the research process by asking questions that are limited in their perspective.
Vl. Limitations
As our approach to the topic has been a holistic one, we recognize that by compressing so many different voices into the same analysis we have lost nuances and depth that could have been captured better by concentrating on only one perspective. We aimed to capture the diversity of views among the wide spectrum of interviewees and include the range of experiences. The interview data is relatively small, and thus, we have not captured all the possible perspectives that could be important to the topic. Yet the purpose of qualitative research is to create empirical understanding of the social reality and to provide data for reflection and discussion.
CONCLUSION
In the end, we return to the vision of patient empowerment that personalized medicine advocates embrace as one of the flagships for the new era of medicine. This ideal depicts patients having an active agency and a clearer voice in the medical ensemble, from research design to data interpretation. While patients would not engage in research design, their input might alter how researchers incorporate correct perceptions of the hope of therapeutic value, rationales for participating, the ways in which being a patient of the researcher might influence the decision to participate, and the different types of relationship between staff and patients. The results could be more patient-friendly or efficient consent processes or even the recognition that patients and practitioners are motivated by the potential of the treatment to be a therapeutic remedy and thus the lines between research and clinical care are intertwined. If this vision is taken seriously, those implementing PM will be faced with the challenge of starting a clinical research methodology that incorporates the patient voice and expectations and the practitioner’s perspectives on personal aspects of care provision, compared to the old way in which the patient stays mostly silent.
In her book Silent Partners,[18] Rebecca Dresser claims that research subjects hold an underutilized, silent perspective on the medical research enterprise. Dresser argues that by considering the perspectives of the actual research subjects, the research communities would be able to make more informed and ethical research decisions.[19] Our study aligns with these arguments and helps prove them by incorporating patient stories into the research and weaving their perspective into the triangle of viewpoints that are represented in the research community. Staff members also may hold perspectives that are often silent in the research design process.
Including different perspectives (the voices that flow into the research triangle) at the beginning of the research design process or at the legislative level when developing the regulations covering research would lead to research processes that are more ethical and accountable to those directly involved, especially those involved in a bodily way, and engaged in both sides of the practitioner-patient relationship.
However, the question of whether the deliberation necessary to improve research can be done likely comes down to whether the medical community is the kind of culture that is willing to seriously include broad perspectives in the research process. According to political scientist Scott Page, cultures of diversity outperform groups of like-minded experts, which makes diversity worth striving for.[20] But, to do this, Page claims first “we have to think of sharing ideas not as giving away the shop, but as collectively building the lever to lift the world.”[21] Curing cancer deserves the benefits of sharing ideas to collectively build that lever.
[1] Cetnar, J. P. & Beer, T. M. (2014). Personalizing prostate cancer therapy: The way forward. Drug Discovery Today 19(9): 1483–1487. doi.org/10.1016/j.drudis.2014.07.006.
[2] Parens, E. (2015). Drifting Away from Informed Consent in the Era of Personalized Medicine. Hastings Center Report 45(4): 16–20. doi.org/10.1002/hast.470.
[3] Pavelić et al. 2016, 8.
[4] Jain, K. (2015.) Texbook of Personalized Medicine. 2nd ed. New York: Springer.
[5] Pavelić, K., Kraljević Pavelić S. & Sedić, M. (2016). Personalized Medicine: The Path to New Medicine. In Bodiroga-Vukobrat N., Rukavina D., Krešimir P. & Sander G. G. (2016). Personalized Medicine. A New Medical and Social Challenge. New York: Springer, 1.
[6] Ibid., 2.
[7] See for example Juengst, E. T., Settersten, R. A. Jr., Fishman, J. R. & McGowan, M. L. (2012). After the revolution? Ethical and social challenges in ‘personalized genomic medicine’. Personalized Medicine 9(4): 429–439. doi:10.2217/pme.12.37; Gaisser, S., Vignola-Gagné, E., Hüsing, B., Enzing, C. & van der Valk, T. (2009). EU policies in personalized medicine-related technologies. Personalized Medicine 6(1): 93–102. doi.org/10.2217/17410541.6.1.93; Brothers, K. B. & Rothstein, M. A. (2015). Ethical, legal and social implications of incorporating personalized medicine into healthcare. Personalized Medicine 12(1): 43–51. doi.org/10.2217/pme.14.65.
[8] Rose, N. (2013). Personalized Medicine: Promises, Problems and Perils of a New Paradigm for Healthcare. Procedia – Social and Behavioral Sciences 77: 341. doi.org/10.1016/j.sbspro.2013.03.092; see also Prainsack, B. (2017). Personalized Medicine: Empowered Patients in the 21st Century? New York: New York University Press.
[9] White House (2015). Factsheet: President Obama’s Precision Medicine Initiative. Press release, January 30. Accessible at [https://obamawhitehouse.archives.gov/the-press-office/2015/01/30/fact-sheet-president-obama-s-precision-medicine-initiative].
[10] Elliot, M., Fairweather, I., Olsen, W. & Pampaka, M. (2016). A Dictionary of Social Research Methods. Online edition. Oxford and New York: Oxford University Press.
[11] Burr, V. (2003). Social Constructionism. 2nd Edition. London and New York: Routledge, 5.
[12] Braun, V. & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology 3(2): 79.
[13] Ibid.
[14] The name of the committee is not disclosed here since it would reveal the location of the study. This is done with regard to the protection of the anonymity of the data.
[15] This was the same nurse who also spoke about being able to give the patients “very very good personal care” (quoted in chapter 3.1.2). This is an example of how statements even in the same interviews can be contrary to each other: first the nurse has told us about giving very good personal care, and later she says that such care is really not possible due to the circumstances and lack of time. This shows that as the thematic frame changes in the course of the interview, even the same thing can look very different from different perspectives.
[16] This is likely to reflect a bias in our data, as the patients not satisfied with their care and untrusting of the staff might not want to participate in PGM research.
[17] See for example a classic article, Appelbaum, P. S., Roth, L. H., Lidz, C. W., Benson, P. & Winslade, W. (1987). False hopes and best data: Consent to research and the therapeutic misconception. The Hastings Center Report 17(2): 20–24; also Lidz, C. W. (2006). The Therapeutic Misconception and Our Models of Competency and Informed Consent. Behavioral Sciences and the Law 24: 535–546. doi.org/10.1002/bsl.700.
[18] Dresser, R. (2017). Silent Partners: Human Subjects and Research Ethics. Oxford: Oxford University Press.
[19] Ibid., xiii; see also Eder, M., Yamoski, A. D., Wittman, P. W. & Kodish, E. D. (2007). Improving Informed Consent: Suggestions from parents of children with leukemia. Pediatrics 119(4): e849-59. doi.org/10.1542/peds.2006-2208.
[20] Page, S. (2007). The Difference: How the Power of Diversity Creates Better Groups, Firms, Schools, and Societies. Princeton and Oxford: Princeton University Press.
[21] Ibid., xviii.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.

