Ice Cold Analysis of the Dachau Experiments
Main Article Content
Abstract
While abhorrent by any standard, the Nazi medical experimentation has become a core illustration of unethically collected data currently being used in scientific research.1-4 Due to the extremes achieved – near-to sub-zero temperatures in investigating hypothermia and its effect on the body – some medical and scientific researchers have claimed it imperative to use the records in order to help individuals in the future.5 This justification is not limited to otherwise unachievable scientific boundaries either; there are calls that the data is just data, the seemingly cold, impersonal collection of numbers and words, while others have oppositely stated that its use not only serves as a reminder of the suffering and injustice endured by those victims, but a way to do good from evil. But this reasoning is wrong. Any loss of knowledge is miniscule compared to the loss in the medical profession if such data is used. By understanding the function of a physician through a Kantian perspective on the Hippocratic Oath, determining the fundamental scientific failures in the Dachau hypothermia experiments, and realizing the moral transgressions under a principlistic paradigm, one can contextualize these bioethical fallacies and work towards creating a morally responsible research framework.
The Oath and its Implications
The Hippocratic Oath serves as prima facie foundation of physician’s morals. As among the first deontological treatises, the Oath expands on a physician’s relation to a patient. Rather than serve a mere mechanical role, the physician, “will use treatment to help the sick according to [their] ability and judgment, but never with a view to injury and wrong-doing.”6 Thus while there is an immediacy to patients as a function of their career, to be a physician is not limited to that function. Instead a physician must transcend this direct professionalism by entirely supporting the beneficial healthcare of a person, whomever they may be.
Yet what constitutes healing instead of harming, helping instead of hurting, and doing good instead of bad? While no answers are directly provided, the Oath places stress on a physician’s disposition to differentiate between right and wrong. 6 But with different cultural backgrounds, societal expectations, and a whole gamut of other variables that a physician must tightrope in their daily life, physicians may differ in their comprehension of good. What is perceived to be beneficent care by one person’s standards may be considered horrendous by another – a gap which the Oath does not elaborate on.
A Kantian consideration can null this ambiguity. By providing an a priori principle that is applicable to all physicians in all circumstances at all times, a Kantian reading can define the rough guidelines of a physician’s obligation to a patient. In accordance with Kant’s first formulation, doctors should, “Act only in accordance with that maxim through which you can at the same time will that it become a universal law.”7 Doctors who stand firm to this maxim cannot see patients as a means to an end, but rather as an end in themselves.8 Whether through research, clinical studies, or direct surgical care, patients are the reason for the profession, not the consequential baggage from it.
This does not mean that the sick are merely subjective ends, however. Rather in the construction of a binding categorical imperative, those that are ill are objective ends with no other alternative than care. One cannot probe or prod unless ensuring it is for the well being of the patient. Thus a true physician acts as though they were treating themselves and operating in a way that would be universally advantageous to all. They consider the individual, even, and perhaps especially, if their research is pertinent to a larger whole. There is no other option. For in following these Kantian dimensions, doctors act wholly human, and in doing so they see the humanity of others reflected in themselves.
The Nazi Political Machine
The Nazi experiments, from chemical castration to phosgene gassing, poison this egalitarian interpretation of the Hippocratic Oath. Key to Nazi Germany was the conception of an unquestioning and unwavering political machine. All individuals were subjected to the eugenically informed policies as a means to “strengthen a biological group on the basis of ostensible hereditary worth despite evolutionary claims.”9 In fact, Hitler was resolute that in order for “the state to act as the guardian of a millennial future…It must put the most modern medical means in the service of this knowledge.”9
A physician’s care was not immune to these intrusions; it instead became the pivot of Nazi biocracy. Through endless appeals to supposedly airtight biology, the romanticism of severe biomedical aspirations, and the unyielding power that doctors were granted in the political sphere, physicians became the veins and arteries of the Nazi lifeblood.10 Approximately 11% of the physician population joined the S.S. compared to 1% of the general German population. Rudolf Ramm of the Medical Faculty of the University of Berlin went so far to propose that, “each doctor was to be no longer merely a caretaker of the sick but was to become a ‘cultivator of genes’ and a ‘ biological solider’”.9
This politically charged personage changed the role of the doctor. From caregiver to care-insurer, physicians acted as both vanguards and mediums for the legitimization of the Nazi medical ethos. Under these eugenic boundaries, no longer was there just a consideration of single individuals; instead a whole population was under a physician’s purview. The function of the physician as implicated in a Kantian reading of the Hippocratic Oath was thus eschewed.9,10In the aftermath, doctors became blind biological barbarians with moral vulnerabilities exposed, moral philosophies skewed, and whose concern was the health of a subjectively chosen population – the Volk – rather than a person and their particular sickness.
Dachau Hypothermia Experiments
This dichotomy in the conceptualization of a Nazi doctor from the one deduced here is important to note, particularly in understanding the ethics behind the research data complied by the Nazi doctors. If physicians are bound to the Hippocratic Oath as it was defined in Kantian terms, then the doctors and medicinal researchers of the Nazi era were anything but physicians. They failed to ensure that the care they provided was care they themselves would want to undergo. Claims of utilizing the most up-to-date science – eugenics – are beside the point. Not because they do not necessarily apply, but because their basis in scientific reasoning is, and was, hackneyed, the progression of racially corrupted thoughts and no more.10 Thus in furthering the analysis of the ethics behind the data collected by these doctors in-name-only, one must understand that what was on display in Nazi Germany was how a profession can fail so completely.
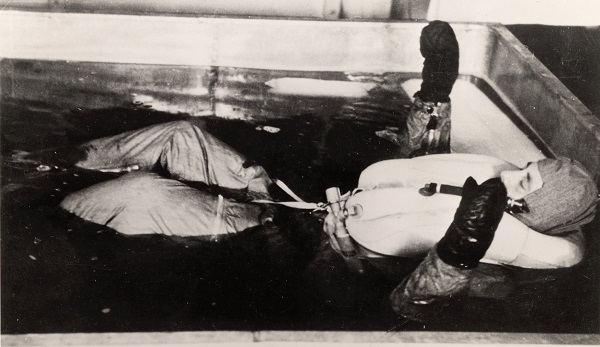
It was from this broken philosophy that the Dachau hypothermia experiments were born. Due to the limited knowledge of the physiological effects of the cold and the frequency at which German pilots often succumbed to it, a national interest into the mechanism of, as well as ways to avoid death from, hypothermia became prevalent.1,2 To satisfy this need, concentration camp prisoners from a wide variety of backgrounds, age groups, and physical conditions were submerged in tubs of freezing temperatures.
Many variables were tested.4,5 Rectal, skin, and gastric temperatures were recorded; blood sugar, concentration of chloride, sedimentation rate, red cell count, plasma proteins, among other blood incidences, were charted; even urinalysis, including the nonprotein nitrogen, viscosity, albumin, sodium, was utilized in the experiments. Additionally, different types of warming methods were developed, from body-to-body contact, warm baths, and candle burning, all of which had varied conclusions.
Ethics in War
While these multitudes of experimental conditions suggest the making of a sound scientific study, the goals of the inquiry must be understood. In Dachau, the experiments were not simply done to satiate experimental curiosity. It was not a progression of knowledge, a dismantling of earlier theories, or an honest, careful probing at the Universe. Instead it was a politically clouded agenda honed in the time of war and littered with theories of racial superiority and inferiority. This purpose, then, could have skewed results for a fixed objective with military weight was the end goal, as opposed to an open interpretation and possibility of alternate hypotheses in a dataset.
This potential for slipshod stringency of the results is only furthered by the suspension of ethics in wartime. While it is easy to decry the Nazi regime for their obvious moral decrepitude, the utility of any data, even if unethically determined, can be viewed in simple terms: will it help win the war; or alternatively stated, if these ends are not pursued, even if they may be malicious, will the war be lost?
To answer the moral dilemma presented, one must refer back to the depiction of the Oath. Only a physician who acts in accordance with it can be rightfully called as such. This means that respect for the patient’s autonomy is guaranteed. Otherwise, the use of a patient in medicinal studies can be seen as nothing more than a banal conclusion in a longwinded study. A non-deontological reading reduces them from human beings who were experimented on to punctuation or a mere footnote of cold insignificance.
Thus a physician can never under any circumstance – even if war – perform such inhumane actions. While unsettling because it may mean the loss of a war, and thus, the loss of even more lives, including the physicians themselves, this is the physician’s moral obligation.
Consider a secondary thought experiment: chemical warfare. Military doctors may be interested of the effects of a new, improvised chemical weapon supposedly owned by terrorists. In this inquisitiveness, they may decide that live populations need to be tested upon. Foregoing ethic boards – or perhaps even convincing them of the very real problem, very likely result of an attack – they test it on prisoners serving life sentences. “It is a requirement in order to save troops,” the researchers say.
While the Nazis and this hypothetical example differ in their definition of a prisoner, the effect is the same: both abuse the physician’s role to the patient. That is, to help, heal, and ensure that autonomy is respected, beneficence – as couched by Boetzkes and Waluchow (2000) – is ensured, and non-maleficence is carried throughout an experiment’s design and implementation. To input any findings that deny these considerations, even if they will save lives, is damage too severe. The loss of a war is small by comparison.
Other Paradigms
But other models, particularly the utilitarian, offer unique insights by creating obligations based solely on judgments of value; 8 that is, one’s actions are morally permitted if and only if they achieve some greater usefulness. Only by the balancing such utility over disutility, often defined in happiness over sadness, and therefore generating the greatest good for the greatest number, can morality be guaranteed.
In this consideration, then, the utilitarian reading of the Hippocratic Oath would state that such research, whether in Dachau or the hypothetical example, would be ethically sound insofar as it ensures that a war is won and more lives are saved.
Unfortunately, problems arise in exactly what utilitarianism prescribes: the consequentialist perspective demands the individuals be killed for another’s benefit. Though it is true that people will die regardless of the outcome in the hypothetical, this prescription of weighing the good of others against someone else seems questionably valuable, not to mention too flexible to individual interpretation. In fact, the utilitarian perspective was the justification behind the Nazification of medicine in the first place.11 Stated simply: the Volk were the future of Germany, and the suffering of the Jews and other minority populations were a necessary evil. To heal the Volk, massacre and experimentation was required. Anything else was worse than death itself. Therefore such reasoning leads to a slippery slope where select populations with power, in this case the military mass of Germany, define what is ethically good and sound.12
The Failure of Dachau
Yet what if the survivors of Dachau, some of those involved in the very experiments themselves, claim that the data should be used as not only a way to commemorate the suffering, but also offer some trace of benefit in an otherwise bleak event?
Different complications result in this novel consideration for it is not a continuation of some past injustice, but an allowance of it by the group directly affected. Consent is therefore obtained, and surely to abuse this agreement is to abuse the abused once again.13 Otherwise stated: unlike the Nazi’s who tried to bury their findings in shame, such allowance does not allow the discoveries to buried again.
Appealing as these considerations may be, the credibility of the data collected must be assessed. In Dachau, the consensus is varied. Berger (1990) maintains the entire experiment, from design to the data to the principle researcher himself, were of little use.4 He noted that the report is riddled with inconsistencies, falsification, and suggestions of fabrication. Others, such as Ivy (1950), have disagreed, claiming that some aspects “were obviously good… and worthwhile.”14
Regardless of what either say, however, the integrity of science, and medicine by extension, is shot in stating that the conclusions hold any clout. Forget that the patients involved are unrepresentative of the larger German population; that is, they were emaciated, used against their will, and were broken, battered, and mistreated if they did not follow orders.1-5 Instead what is central to scientific inquiry – more than the collection, analysis, and presentation of some form of data – is reproducibility.13 By their very nature, the Dachau experimentations are irreproducible. The claims cannot be challenged, only postulated upon; the results cannot be replicated, only assumed to be true within degrees of error. Thus, they lack the scientific rigor that is otherwise necessary to be truly defined as science.
The Broader Scientific Implications
Moreover, a truly comprehensive study is only benefited, not deterred, by ethical treatment.8 A balanced research relationship encourages disclosure, trust, and awareness of findings and their implications. Denying this denies the justice in recognizing a patient’s vulnerability, the holistic approach to inquiry with its multifaceted concerns, from a person’s personal background, medical history, beliefs, and opinions, and the two-fold narrative of healthcare. With an ethical model, those experimented on can comment on unique aspects of a study and physicians and researchers alike can mend the design as is required and suggested to produce the best results.
However, what if the Nazi doctors discovered a cure to cancer? On intuition alone, there seems no harm in allowing the dissemination of this knowledge; in fact, it seems by not bringing this knowledge to the fore, more harm will result. However what is clearly evident that no physician, as it was defined, is justified in reducing subjects to their ends, whatever they may be. Doing so encourages further unethical experimentation that rides a slippery slope to scientific martyrdom. And selecting martyrs is not science’s business. Neither is it the physician’s.
More importantly is that such unethical experimentation may be supplemented by ethical treatment. Take Dachau again. Similar findings were discovered in animal studies, and these may be extrapolated to human cases.2 And if this is not a possibility, then the alternative is much less dark: informed consent may be given by the patients and this allows a more fruitful discovery to occur.
In this way, there are always better, more reasonable means to the spirit of invention. That is science’s testament. It is what the scientific methodology ultimately strives for: putting humanity in the inhumane. To do otherwise, and to participate in unethical medicinal practice, is to deny the very construction of science and medicine.
Conclusion
Unethical practice and research of medicine should never be pursued for its own end. The loss of autonomy, the warping of a physician’s both moral and vocational duty, the disregard of trusting relationships, the reduction of patients from research subjects to research objects, and the skewing of beneficence necessary to achieve the supposed end is not worth the result, no matter how lucrative and beneficial it may seem. The Kantian philosophy, as well as the framework of principlism, cries for research of a higher moral standard. Because while under the utilitarian lens of science all types of research can be used to rationalize saving lives, what must not be asked is what is the end result, but instead, what is the cost to get there – whether that be to the physician, the patient, and humanity as a whole.
REFERENCES
1. Dyal, E. Nazi Medical Experimentation: Should the Data Obtained be Used? Southern Illinois University Theses, 2000.
2. Pozos, R. Nazi Hypothermia Research: Should the Data be Used? Military Medical Ethics, 2, 1991.
3. Caplan, A. When Evil Intrudes. The Hastings Center Report, 22, 1992.
4. Berger, R. The Dachau Hypothermia Experiments. The New England Journal of Medicine, 322, 1990.
5. Post, S. The Echo of Nuremberg: Nazi data and ethics. Journal of Medical Ethics, 17, 1991.
6. Hippocrates. Trans: Jones, W. H. S. Oath. Cambridge: Harvard University Press. 1923. Print.
7. Kant, I. Trans: Wood, Allen. Groundwork of the Metaphysics of Morals. Boston: Yale University Press. 2002. Print.
8. Introduction; Readings in Health Care Ethics. Elisabeth Boetzkes and Wilfrid J. Waluchow eds. Broadview Press 2000.
9. Lifton, R. The Nazi Doctors: Medical Killing and the Psychology of Genocide. United States: Basic Books. 2000. Print.
10. Colaianni, A. A Long Shadow: Nazi Doctors, moral vulnerability, and contemporary medical culture. Journal of Medical Ethics, 38, 2012.
11. Dixon B. Citations of shame. New Scientist. 1985; 105: 31.
12. Nichols, S. Mallon, R. Moral Dilemmas and Moral Rules. Cognition, 100, 2006.
13. Rob, A. Eisenhauer, L. Wynaden, D. Ethics in Qualitative Research. Journal of Nursing Scholarship, 33, 2000.
14. Mitscherlich A, Mielke F. Doctors of Infamy: The Story of the Nazi Medical Crimes. New York: Henry Schuman; 1949.