Apology Laws and the Doctor-Patient Relationship
Main Article Content
Abstract
In 2000, the Institute of Medicine (IOM) published “To Err Is Human: Building a Safer Health System,” a report on the woeful state of patient safety in American hospitals.1 This alarming study not only forced the medical establishment to acknowledge the extent and consequences of human error; it spurred states to look for ways to better protect their citizens from medical mistakes. One intriguing suggestion was to allow healthcare providers to own up to those mistakes. Conflict resolution scholars, hospital administrators, and state governments (everyone who had an interest in improving the IOM statistics) agreed that if errors could be discussed in the open, they could be freely and thoroughly analyzed. Such transparency might expose the reasons for the mistakes, which could lead to prevention strategies.
Traditionally, medical error is dealt with in the courts, and the threat of litigation serves as a deterrent to doctors. The new, post–IOM report suggestion also involved the legal system, but in this case it didn’t include the courts hearing malpractice cases but rather state legislatures granting immunity to certain expressions of apology by statute. This new approach was implemented in 2003, when Colorado enacted the country’s first “apology inadmissibility law.” Other states soon followed suit.

The new laws were designed to reduce medical error and malpractice litigation, but bioethicists hailed them too. Bioethicists hoped that the apology laws, even in the wake of adverse outcomes, could serve to maintain the continuity of care that is part of humane medical attention. An atmosphere in which physicians could openly admit mistakes, express condolences, and perhaps discuss reparations without fear of being sued would mean patients or their families wouldn’t have to go to court to discover what had gone wrong with their loved ones’ medical treatments. The doctor could preserve his own dignity and autonomy as well, by honoring his professional and ethical mandates to act in his patient’s best interests. Bioethicists saw in state apology laws a chance to prevent the devolution of the relationship of doctor-patient into that of defendant-plaintiff.
Yet despite state efforts to protect doctors, the moral promise of the apology laws was never fulfilled. To the contrary, as a review of the laws reveals, the doctor-patient relationship couldn’t be a concern of the apology statutes because of the way the statutes were crafted in the first place.
•
“A pivotal development in American legal and medical practices may have occurred quietly in Colorado last year,” wrote Jonathan Cohen, a law professor and dispute resolution scholar, in spring of 2004. “It took the form of a change in Colorado’s evidence code.”2 Cohen was writing about CRS §13-25-135: Colorado Law Governing Apology for Unanticipated Outcome in Medical-Legal Proce[e]ding,3 the country’s first “apology inadmissibility law.” (Six states already had statutes on the books exempting expressions of benevolence or sympathy from admissibility as evidence—Massachusetts was the first, in 1986—but Colorado’s law was the first to specifically exempt physicians’ admissions of fault.4)
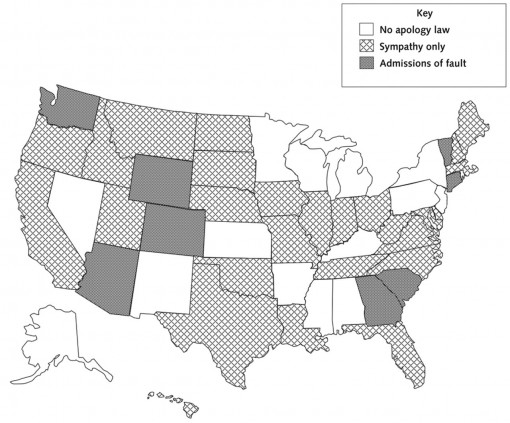
The practice caught on, and, by mid-2013, 37 states and the District of Columbia had enacted some form of apology inadmissibility law.5 Although all of them provide protection for simple expressions of sympathy, most of the statutes specify to whom the expressions can be made. In addition to defining what is inadmissible as evidence, the laws dictate what the apologies or benevolent gestures can “relate to.” For instance, 14 states protect expressions of sympathy only if they spring from cases in which there’s been an “unanticipated outcome” during medical care. Five states allow expressions of sympathy only if an adverse outcome is the result of an accident. Hawaii protects expressions of sympathy when the sympathizer is a participant in the event that elicited the expression, and Iowa exempts statements of condolence or compassion for cases in which the adverse outcome results from a breach in the “applicable standard of care.”
A few statutes impose interesting additional qualifications. West Virginia’s inadmissibility law is restricted to “civil action, including arbitration, mediation, or alternative dispute resolution proceeding” (emphasis provided). Texas’s law requires that expressions of compassion or commiseration “emanat[e] from humane impulses…or a general sense of benevolence” but adds that a “communication including an excited utterance as defined by Rule 803(2) of the Texas Rules of Evidence, which also includes a statement or statements concerning negligible or culpable conduct pertaining to an accident or event, is admissible to prove liability of the communicator.”
The breadth and variety of restrictions and qualifications to the laws reflect the diligence that went into drafting them. Yet for bioethicists who had hoped that apology laws would benefit the doctor-patient relationship by removing the threat of litigation, the upshot of the laws has been disappointing. They remain focused on reducing the exposure of states and their medical institutions to civil action and potential penalties; instead of including the doctor-patient relationship within the scope of the legislation, the laws have achieved the opposite.
Bioethicists interested in the ethical implications of apology laws will be alarmed to learn that fewer than a quarter of the statutes allow physicians to take responsibility for their actions: For an apology to be sincere, after all, it must include both the transgressor’s acknowledgement of wrongdoing and an expression of remorse. Without an admission of fault or other recognition of responsibility for error, an apology is incomplete—it’s more like a politician’s acknowledgment that “mistakes were made.”
Critics of apology laws have noticed that the apologies protected by the statutes are neither sincere nor complete. Ethicist and lawyer Lee Taft wrote “Apology Within a Dialectic” in reply to an empirical study of the role of apology in legal settlements.7 He takes issue with the notion of legislating apology at all, precisely because the laws can lead to incomplete, insincere expressions. He believes utility to be the real motivation behind the inadmissibility laws, and thus they’re liable to discount the crucial, moral component of a sincere apology. Even if apology laws are proven to reduce malpractice cases, Taft maintains, and even if they improve patient safety, they would still fail to “adequately address the moral harm of legislative protection for apology.”8 Put another way, the “efficacy of apology is not dependent on its admissibility [in court].”9 Rebecca Dresser agrees, writing in “The Limits of Apology Laws” that inadmissibility statutes “will achieve a positive ethical outcome only if they are accompanied by full disclosure and fair compensation.”10
Apologies that don’t include admissions of fault are also one-sided. By failing to own up to his role in causing harm, the transgressor fails to acknowledge the victim’s moral status in the equation. Without that acknowledgement, the harmed party is little more than the passive recipient of legally approved remorse. On the American Medical Association’s (AMA) chart of state inadmissibility laws, patients or their families are there to receive legislated expressions; they play no active role in the process.11
Nancy Berlinger is thinking in this vein in “Avoiding Cheap Grace: Medical Harm, Patient Safety, and the Culture(s) of Forgiveness.” She writes that, in partial apologies, the injured party is “pushed out of the frame, while the person who has made the error is forgiven without any assurance that the relational actions traditionally described as confession and repentance have taken or will take place.”12 For Berlinger, a partial apology is one in which forgiveness is not sought by the transgressor but is instead bestowed upon himself by himself. This conception is notable for its absence of moral consideration of the injured party. On more practical grounds, writes law professor Anna Mastroianni and colleagues in their survey of the impact of apology laws on malpractice litigation, “lawsuits that protect only expressions of sympathy and explanation may make for awkward communications, as it may be difficult to explain an error without discussing the different but closely related issues of responsibility and fault.”13
To the bioethicist, then, the more than 75 percent of apology inadmissibility laws currently on the books are not about apology at all, but rather a circumscribed notion of it.
•
If most apology inadmissibility laws aren’t really about apology, then they must be about something else. One reasonable candidate would be the continued protection from civil action for adverse medical outcomes that result from physician error. So even though the apology legislation movement gained momentum after the IOM report, the way the laws have been written indicates that the move to shield expressions of physician mea culpas was never sparked by concern for patient safety to begin with. Instead, the laws seem to exist to better protect medical providers from legal exposure at very little expense. (As Cohen notes, the cost of enacting laws that protect healthcare providers’ expressions of sympathy is pretty much “nothing.”14)
Taft agrees that apology laws are more about lawsuits and less about encouraging an honest dialogue between doctor and patient. He takes issue especially with the idea that an adversarial legal system can be retrofitted to both reduce malpractice suits and accommodate a moral relationship like that of doctor and patient, writing that the “risk of subversion arises whenever we transcribe moral processes into systems that are primarily adversarial.…15 This harm rises dramatically when one extracts components of moral processes and inserts them into utilitarian schemas”16—such as those designed to improve patient outcomes and reduce instances of malpractice suits. Flauren Fagadau Bender, an attorney specializing in health law, advises physicians who are thinking about extending apologies to patients to check with an attorney first.17 That is, before a doctor decides to act in accordance with a law that was created expressly to encourage him to act without fear of being sued, he first should run his decision by Legal.
The undercurrent of the ethical objections to inadmissibility laws is the simple fact that when a physician inadvertently injures a patient, he harms someone with whom he has created a uniquely intimate relationship. The physically and emotionally vulnerable patient entrusts her well-being to her doctor. If he harms her, and chooses to override his humane (and human) impulse to apologize in favor of checking first to see if such an apology comports with his institution’s legal protocol under state law, he withdraws from his relationship with her; he has turned his attention to his own needs rather than his patient’s. His concern now is with his new role as potential respondent to litigation. With this shift in priority, the doctor has effectively abandoned his patient.
•
Of course, state lawmakers never claimed to be trying to inject a dose of morality and humanity into the world of malpractice litigation when they drafted the apology statutes. The AMA calls them Apology Inadmissibility Laws, after all, and its state-by-state overview is titled a “Summary of State Legislation.” Three states and the District of Columbia are quite up-front about their purpose in enacting apology laws when they restrict the domain of expressions to cases in which civil action has already been undertaken.
Also, given the size and complexity of the U.S. medical system, it isn’t surprising that a solution to the problem of fatal medical error would include bottom-line considerations. Early last year, journalist Steven Brill provided an exhaustive investigation into how Big Medicine operates in the U.S.18 Anyone reading his descriptions of the often inscrutable world of the business side of medicine would easily understand why such ethical considerations as the doctor-patient relationship would play second fiddle to financial concerns in any attempt to improve the system. Add in the cost of malpractice insurance and lawsuits, and hospital administrators and state legislators would be deemed fiscally irresponsible if they undertook any kind of medical system overhaul without keeping the costs of malpractice litigation firmly in mind.
Still, the laws arose against the backdrop of the IOM report’s dismaying statistics on patient mortality. They were seen as a potential solution to medical error, and because medical error necessarily entails a doctor to commit the error and a patient to be harmed by it, ethicists had good reason to believe the laws might include an ethical component—that the apologies covered by the statutes would be real ones offered sincerely and openly by remorseful doctors to their suffering patients. When Cohen wrote about that first apology law in Colorado, he welcomed it as an opportunity to “promote an open, trusting and care-giving relationship following medical error.”19 Similarly, Dresser thought the statutes had the potential to “advance other ethical objectives,” such as enabling doctors to “tell the truth and promote patients’ best interests.”20
Yet even if the intent of the laws was always to reduce the number and impact of malpractice claims, that doesn’t mean that lawmakers and hospitals are justified in letting the doctor-patient relationship go by the wayside. Without doctors and patients, the medical enterprise wouldn’t exist. Their relationship is the foundation of both medicine and bioethics. A solution to the problem of patient safety, then, will necessarily have to be an ethical one.
The legacy of the apology inadmissibility law movement has turned out to be a raft of statutes that suggest new ways of protecting the medical establishment from its own mistakes. The unintended consequences of these seemingly well-intended laws are doctors who can’t apologize for harming their patients even if they want to and injured patients who’ve been abandoned by their caregivers.
REFERENCE NOTES
1. To Err Is Human: Building a Safer Health System, ed. L. Kohn, J. Corrigan, M. Donaldson (Washington: National Academy Press, 2000), p. 26.
2. J. Cohen, “Toward Candor After Medical Error: The First Apology Law,” Harvard Health Policy Review 5, no. 1 (Spring 2004), p. 21.
3. CRS §13-25-135: Colorado Law Governing Apology for Unanticipated Outcome in Medical-Legal Proceeding.
4. J. Cohen, “Toward Candor After Medical Error: The First Apology Law,” p. 21–22.
5. “Apology Inadmissibility Laws: Summary of State Legislation,” American Medical Association Advocacy Resource Center (2012).
6. Ibid.
7. J. Robbennolt, “Apologies and Legal Settlement: An Empirical Examination,” Michigan Law Review 102, no. 3 (Dec. 2003), p. 460–516.
8. L. Taft, “Apology Within a Moral Dialectic: A Reply to Professor Robbennolt,” Michigan Law Review 103, no. 5 (Mar. 2005), p. 1011.
9. Ibid.
10. R. Dresser, “The Limits of Apology Laws,” Hastings Center Report 38, no. 3 (2008), p. 7.
11. “Apology Inadmissibility Laws: Summary of State Legislation.”
12. N. Berlinger, “Avoiding Cheap Grace: Medical Harm, Patient Safety, and the Culture(s) of Forgiveness,” Hastings Center Report 33, no. 6 (2003), p. 34.
13. A. Mastroianni, M. Mello, S. Sommer, M. Hardy, T. Gallagher, “The Flaws in State ‘Apology’ and ‘Disclosure’ Laws Dilute Their Intended Impact on Malpractice Suits,” Health Affairs 29, no. 9 (2010), p. 1611.
14. J. Cohen, “Toward Candor After Medical Error: The First Apology Law,” p. 24.
15. L. Taft, “Apology Within a Moral Dialectic: A Reply to Professor Robbennolt,” p. 1016.
16. Ibid., p. 1014.
17. F. Fagadau Bender, “‘I’m Sorry’ Laws and Medical Liability,” American Medical Association Journal of Ethics 9, no. 4 (2007), p. 302.
18. S. Brill, “Bitter Pill: Why Medical Bills Are Killing Us,” Time 181, no. 8 (Mar. 4, 2013).
19. J. Cohen, “Toward Candor After Medical Error: The First Apology Law,” p. 22.
20. R. Dresser, “The Limits of Apology Laws,” p. 6.


 PDF
PDF