The Use of Mitochondrial Replacement in IVF A Call for Expansion
Main Article Content
Abstract
In 1978, the United Kingdom made history with the birth of the first baby conceived with the help of In Vitro Fertilization (IVF). Since then, IVF has helped countless people start a family who would otherwise have been unable to conceive. Thirty-six years later the UK is again announcing breakthroughs in the science of reproduction. Last fall, scientists in the United Kingdom announced that they would use mitochondrial replacement in the IVF process to remove the chances of a child being born with a mitochondrial disease. This advance in reproductive technology has yet to be accepted by the rest of the world, where regulations on artificial reproductive technologies may need to be amended for its use to be legalized.
Mitochondrial DNA and Diseases
During the normal process of fertilization, a potential child will receive equal amounts of nuclear DNA from its mother and father, while the entirety of the mitochondrial DNA is received from the mother. The majority of a person's genetic makeup is held within the nuclear DNA, whereas the mitochondrial section contains only 37 genes. Mitochondrial DNA, for a large part, provides power for cells to convert food into energy. The problem is that mitochondrial DNA can sometimes contain mutations that lead to mitochondrial diseases. These diseases can be severe, causing damage to areas of the body including the brain, heart, liver, and kidneys. Some are life threatening while others can lead to cognitive developmental delays, blindness, muscle pain, or seizures to name a few symptoms. If a mother has mutated mitochondrial DNA, it is a certainty that their child will be affected. Mitochondrial diseases effect up to one in every 6,000 children born in a year.
The Importance of Mitochondrial Replacement
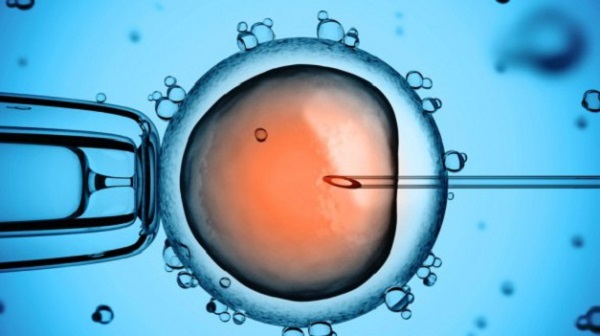
Mitochondrial replacement removes the diseased mitochondrial DNA of the nuclear DNA mother and replaces it with the mitochondrial DNA of a second, donor female. This is done in hopes of preventing the potential child from developing a mitochondrial disease, or passing such a disease down to future generations. This procedure has shown to be effective in primate trials. In 2009 it was announced that four macaques that had the mitochondrial replacement procedure done to their embryos were born healthy and without deformity.
The importance of such a medical breakthrough cannot be denied, especially when it has the potential to save the lives of children, and prevent them from having to grow up disabled. With approximately 134 million people being born a year, this has the potential to improve the lives of about 22,000 children. Such technology has an important global impact, and should be available in other countries besides the United Kingdom; however, the ethical considerations of its use need to be addressed.
Ethical Considerations
A common ethical issue that arises with reproductive technologies is the fear that the use of this new technology will lead back to an era of eugenics, or that in the near future babies will be designed to have certain preferred genes over others. Mitochondrial replacement is altering the normal DNA structure of a female's egg by replacing some of that DNA with an entirely different person's genetic material. Might this lead to parents selecting what specific characteristics of the mitochondrial DNA be used? Or potentially will "mad scientists" experiment on human embryos by inserting the mitochondrial DNA of another mammal?
While the abuse of any technology should never be disregarded as impossible, the mitochondrial replacement procedure should be considered a low threat for opening the door to eugenics and designer babies since it does not allow for the selection of specific genes; it simply replaces one set of mitochondrial DNA for a non-infected set. Besides, the genetic information within mitochondrial DNA is only 37 genes. Outside of being born without a mitochondrial disease, that is hardly enough genetic information to have an impact on the qualities and characteristics of the child-to-be.
Another issue that mitochondrial replacement raises is an injustice in the distribution of services. This technology has only been allowed by the United Kingdom for the time being, which gives the UK the ability to set the cost of such a procedure, as well as who will have access to use it. This can create worldwide discrimination and feelings of injustice if the United Kingdom decides to put a high price tag and limitations on who can receive mitochondrial replacement.
Such worries can be alleviated, though, if the use of mitochondrial replacement is expanded to other countries. This would ensure that a person could not be prohibited from accessing such services based on the country they live in. The financial burden is another issue, however, but one that may not be as extreme as some may think. Mitochondrial replacement is not necessary for everyone who is using IVF services, only those who carry mutated mitochondrial DNA. This in itself will cut down on the potential group of people who will feel a financial burden because of such a procedure. It can also be assumed that over time, like current IVF, some insurance companies will cover the cost of the additional practice of mitochondrial replacement. To do so would be cost-effective for insurance companies in the long run since they would not have to worry about covering any medical costs related to mitochondrial diseases that would develop without having mitochondrial replacement done.
Lastly, opponents to mitochondrial replacement may argue that such a procedure is discriminatory towards people with disabilities. Much like the debate that has arisen over testing for Down's Syndrome, opponents may argue that not all mitochondrial diseases are life threatening and the use of this procedure is stating that a life with a disability is not worth living. Many people with Down's, blindness, hearing impairment, and other debilitating but not deadly diseases go on to live happy and fulfilling lives. Such a procedure will lead to increases in discrimination against those with such disabilities since these diseases now can be thought of as curable.
In response to such an argument, I would emphasize that this procedure is not mandatory or compulsory. Those parents who seek out such a procedure are doing so because they believe it is what is best for the future of their child. Parents are given the ability to make decisions for their children who cannot yet make their own autonomous judgments, and mitochondrial replacement would be yet another area where such decision making is acceptable. The science does not advertise itself as a way to prevent disabled children; it is a way to prevent children from developing a specific set of diseases.
Ethical Analysis
Having discussed some of the major ethical issues related to mitochondrial replacement, the only thing left to determine is if a new technology such as this holds up under the bioethical principles of research and clinical practice. Some will argue that mitochondrial replacement does not meet the standard of autonomy since children are not able to choose if they would like such a course of action done to them. In general, though, children do not get to choose their genetic composition when conceived naturally. Having 37 genes changed will have no great impact on the child's development or character, and the selection of any specific 37 genes could not be controlled by the child under normal circumstances anyway. Additionally, in general and when it is in the best interest of the child, parents are allowed to make autonomous decisions for their children when that child is too young to make decisions for themselves. Preventing a child from being stricken with a disease would fall under this category, and is the duty of all parents.
In regards to issues of justice, not everyone will be able to afford such a process, but on the other hand, not everyone needs to use such a process to begin with. Currently, mitochondrial replacement may not meet the principle of justice but the way to ensure that those who do need access to mitochondrial replacement will eventually have equal access to it is by increasing its use, not stopping use altogether. With further developments, the science will improve and insurance companies will hopefully start coving the cost of the procedure.
Lastly, as with all new technologies the risks and benefits of such technology must be assessed. There may be several risks associated with this process. The embryo may be damaged during either the mitochondrial replacement or IVF procedure, or some of the nuclear mother's mutated mitochondrial DNA may not be successfully removed from the egg. These risks can lead to the child being born with some dysfunction despite having gone through mitochondrial replacement. There is also the fact that the long-term effects of mitochondrial replacement are not yet known. The long-term effects can be assumed low though since the mutated mitochondrial DNA is replaced with healthy DNA and not just removed.
These risks, however, do not outweigh the benefit of being able to prevent children, and future generations, from being born free of mitochondrial diseases. The purpose of medical science is in part to improve peoples' lives. Few would argue that a life without disease would not fall under the category of improvement. Since mitochondrial disease can effect a child born in any region of the world the only ethical response is to expand such technology to other countries outside of the United Kingdom that have the resources and capability of using such reproductive technology.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.