Compulsory COVID-19 Vaccination? Only as a Policy of Last Resort
Main Article Content
Abstract
Photo by Daniel Schludi on Unsplash
The debate regarding the limits of individual liberty and the state’s obligation to promote the common welfare and to protect its citizens is too important to be left to extremists. As more vaccines make their way through Phase III trials[1] and the question of compulsory vaccination presents itself, leaders must address the short- and long-term implications of requiring a specific medical intervention (vaccination) as a condition of community membership[2] versus as a condition of participation in school, work, or other activities. Transparency and openness to compromise are paramount. Broad buy-in on policy which touches such a fundamental human interest, the right of individuals to control their own bodies, is crucial to restore or ensure continued trust in science and American institutions and to prepare the country to combat future problems. This paper argues that universal compulsory vaccination (by state or county) should be implemented only as a policy of last resort. Public health officials must first weigh all reasonable alternatives, including educational initiatives, tax credits (rather than penalties), and variously-formulated requirements for vaccination of subsets of the population as a condition of participation in public activities.
HISTORY
In 1902, the Board of Health of Cambridge, Massachusetts, using authority delegated to it by the state legislature, required smallpox vaccination or revaccination for all healthy residents above the age of 21. Those who refused were subject to a five dollar per day fine. A pastor by the name of Henning Jacobson was prosecuted, fined, and ultimately ordered committed for refusing to pay that fine. In Jacobson v. Massachusetts, Justice John Marshall Harlan wrote the majority opinion for a seminal 7-2 Supreme Court decision upholding the right of the state to compel vaccination under certain circumstances.
Underpinning the Court’s conclusion was a tense and uncertain compromise between the tenets of social-compact theory and theories of limited government.[3] Although Harlan wrote that the constitution guaranteed no “absolute right in each person to be, at all times and in all circumstances, wholly freed from restraint,”[4] he underscored that the state’s police powers were limited. The state must always (1) consider the necessity of their exercise, defining its objective as narrowly as is feasible, (2) use “reasonable means” to pursue that objective, (3) impose only burdens that are proportionate to the expected benefit, and (4) avoid inflicting “cruel and inhuman harm” on any person.[5] Harlan implied that state legislatures were to have wide discretion to deliberate these issues and perform benefits/burdens calculations themselves.
Jacobson legitimized compulsory vaccination legislation then on the books in 11 states, but such legislation was seldom used. Most states vigorously promote vaccination for various diseases through educational initiatives or require it for students seeking to enroll in public school (always with medical and usually with religious or philosophical exemptions) or for certain subsets of the population, like healthcare professionals working in select hospitals and nursing homes.[6] Mandatory public school vaccination has withstood court challenge,[7] but mandatory vaccination of healthcare professionals, when no non-medical exemptions are granted, is of ambiguous legal status.[8] Since 2000, some states have passed versions of the Model State Emergency Health Powers Act (MSEHP), granting their governors the authority to declare public health emergencies and thereafter to compel vaccination of the public, using the National Guard if necessary.[9] However, no qualifying crisis scenario presented itself until this year. Governors contemplating COVID-19 vaccination requirements are likely first to develop plans which would make vaccination a condition of participation in various activities, a strategy that, although still controversial, is not the primary subject of this paper. It is unlikely that the federal government would get involved. Though it imposes some vaccine requirements for those wishing to immigrate or join the military, it has never established broader vaccination policy, and it is unclear whether it could use its authority, e.g., under the constitution’s Commerce Clause, to do so.[10]
PRACTICAL AND ETHICAL CONSIDERATIONS
After FDA approval of a vaccine for COVID-19, it is conceivable that some states, or some legislators within them, spurred on by medical and other commentators,[11] will wish to compel vaccination not only of children in public schools or of healthcare professionals working in certain settings, but of at-risk groups or of all citizens under their jurisdiction. While it is extremely unlikely that they would authorize the use of force, they might impose fines or tax penalties, as the Board of Health of Cambridge, Massachusetts did at the turn of the 20th century. Such moves are likely to be challenged in court, and if they make their way to the Supreme Court, it is not altogether clear how the Court would rule or whether its ruling will be delivered in time to be relevant. Compulsory vaccination of specific groups, e.g., the elderly or those living in crowded housing or in high-spread neighborhoods, who might be disproportionately Black or Hispanic, [12] could be struck down on the basis of the 14th Amendment’s guarantee of equal protection, which Jacobson never addressed. Although Jacobson has been cited in more than seventy other cases, most dealing with other non-health- or health-related uses of police powers,[13] and is well-established precedent, the Court has acknowledged several other rights in the intervening years which might lead it to overturn Jacobson. These include a right to privacy[14] and a right to refuse unwanted medical treatment.[15] Although it has always balanced these rights against state interests,[16] which certainly include preventing the spread of disease, the communitarian spirit of the Progressive Era has given way to a polarized electorate that includes growing numbers of uncompromising liberty enthusiasts. All fifty states have vaccination mandates for school attendance and several states mandate vaccines for healthcare workers demonstrating Jacobson’s precedent has survived the development of privacy rights and rights to be free from unwanted bodily intrusions in the healthcare context. The issue of whether Jacobson has survived legal progress to the degree that universal compulsory vaccination (rather than school or workplace mandates) would be acceptable remains unanswered. The Court now includess several self-described staunch defenders of individual liberty and autonomy who may not give as much weight to public health measures that are seen to infringe upon fundamental freedoms.[17]
But even if the Court were to uphold the essence of Jacobson, the particulars of the case before it would determine whether compulsory COVID-19 vaccination could proceed. The current Court might defer less to the determinations of state or local public health agencies and apply higher or different standards for necessity, reasonable means, proportionality, and avoidance of “cruel and inhuman harm” than did Harlan’s majority. On the basis of fairness and minimizing individual burden, it could determine that compulsory vaccination is permissible only when the vaccine is offered at no expense at properly-spaced clinics or other centers, which would be infeasible for many states. The Court’s recent backing of a religious challenge to limits on gatherings that New York imposed in response to a second surge of COVID-19 infections in October is a tangible indication that the Court might require states to offer religious or philosophical exemptions.[18] The Court may strike down a universal compulsory vaccination policy if it does not believe that a state has done enough to promote voluntary vaccination first, especially considering the additional tools states have at their disposal today. Given the probable impact on public order or possible setbacks for vaccines if something should go terribly wrong, a decision against broad compulsory vaccination on the grounds that other policies were not exhausted first may be beneficial to social stability.
It is also important to remember that vaccines do carry some risks – hence the existence of a National Vaccine Injury Compensation Program.[19] Many bioethicists downplay the risks of vaccination for the non-immunocompromised. Alberto Giubilini goes further. He has compared the decision not to be vaccinated to tax evasion and has justified compulsory vaccination on the basis of fairness: shared risk for shared reward, rather than harm prevention.[20] But even if his argument demonstrated that compulsory vaccination were morally permissible or even morally obligatory, it does not show that compulsory vaccination is good public policy, especially when the vaccine in question is new. I argue that the consequences (loss of social cohesion and trust in the scientific community) would outweigh the benefit of reduced viral spread.
That opposition to vaccination is growing[21] and that more than 40 percent of Americans indicate they would not consent to receive even a cost-free COVID-19 vaccine[22] should be the starting point for government vaccination policy. While the state has a responsibility to educate its citizens on issues pertinent to the public welfare and to override them when the consequences of not doing so are likely to be disastrous, it must first make good-faith attempts to address all concerns voiced by its citizens, making accommodations when possible. A minority should not be ignored simply because it is a minority, and if it is a large minority, the implications of overriding it for social cohesion and for democracy, must be given attention. Some warn that the country is more polarized now than at any time since the Civil War,[23] and in the age of mass media and social media, compulsory vaccination is likely to become a flashpoint, like mask mandates and social distancing before it.[24] But unlike those mandates, universal compulsory vaccination threatens or comes close to threatening a fundamental liberty interest and is likely to encounter even fiercer resistance, especially if the mandate comes from the federal government.
Although Joe Biden’s victory in the presidential election may improve public confidence in a vaccine and in the FDA, it is possible that some will still be uncomfortable with how quickly a COVID-19 vaccine was developed relative to other vaccines.[25] They may prefer others take it before they do, particularly if the vaccine receives emergency use authorization.[26] Pluralism and democracy are virtues, and it would be unethical to disregard the concerns of this group, especially as they are not altogether unreasonable. Circumstances may enable broad circumvention of this issue. Vaccine roll-out will not be instantaneous, and demand for it may be high enough that governments must use distribution prioritization schemes (granting access to healthcare workers, the elderly, other essential workers, etc. first). Over time, if these populations do well, others may become convinced and choose to be vaccinated.
Alternatively, individual states or the federal government might attempt to push them along, e.g., by denying them access to post offices, schools, or other public property or requiring them to quarantine if they travel but have not received a vaccine, that is, requiring vaccination as a condition of participation in public activities. Whether this will bring the total number of vaccinated people up to the level necessary to achieve herd immunity will depend on how effective the vaccine is and whether its protection is permanent.[27] Paradoxically, if the vaccine is less effective or boosters must be given, more people will need to receive it, but the courts, performing a risk/benefit analysis, are less likely to uphold a mandate. It would also be less ethical for them to do so, as the potential for harm and burden imposed would be greater.
Finally, many people who support or are ambivalent to vaccination in general will oppose compulsory vaccination for COVID-19, either because they oppose the exercise of this type of state power in principle or because they do not believe the necessary threshold has been met. These people may worry that the state will begin to implement measures like compulsory vaccination when no crisis exists or fail to appropriately circumscribe the limits of what constitutes a crisis. As a recent example of executive overreach, President Trump once declared a national emergency over immigration at the southern border in order to bypass the legislature and free up spending for a wall (a campaign promise).[28] Although the WHO, itself not immune from political influence, publishes parameters for staging pandemics,[29] it does not (and cannot) describe a uniform policy on what precise levels of spread, hospitalization, or mortality merit what type of response. There is no law requiring governors or presidents to declare public health emergencies only when case-specific WHO or similar criteria are met.
SUMMARY & RECOMMENDATIONS
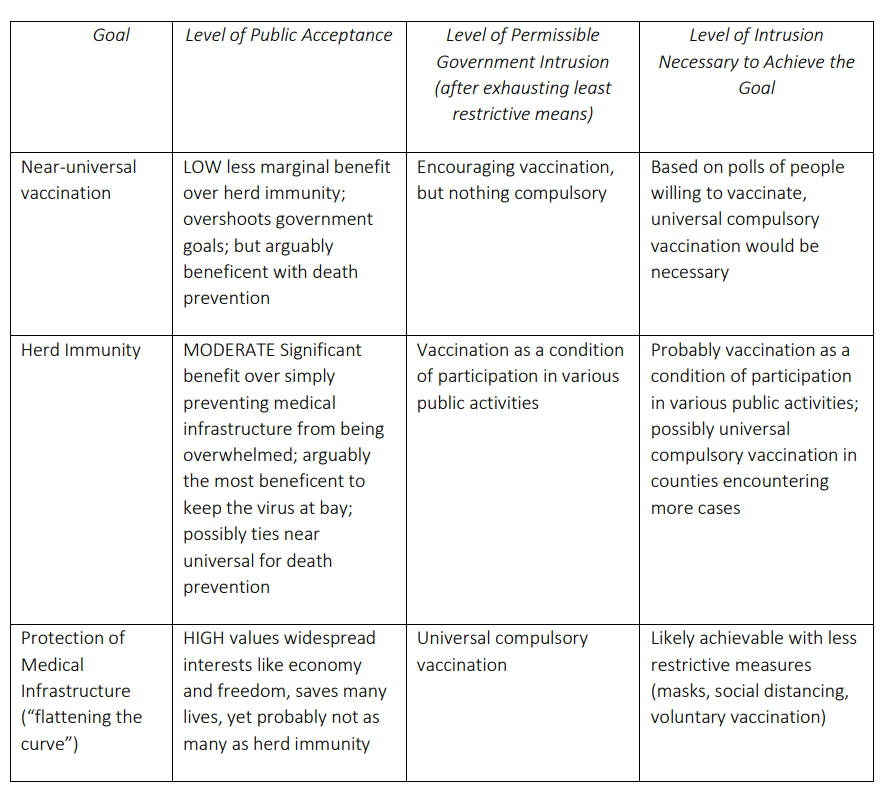
It would be difficult to formulate a sustainable, cost-effective universal compulsory vaccination policy that stands up to court scrutiny and strikes a balance between autonomy, respect for bodily integrity, and public health that most people will accept and that does not further marginalize disadvantaged groups. In light of this, I argue that states should have tiered goals for vaccination and use interventions of varying strength and scope to achieve each, communicating transparently to the public and giving heavy weight to people’s concerns.
The marginal benefit of pursuing each, more ambitious goal decreases as the less ambitious goals that are subsumed into them are realized. The harms associated with pursuing them may be great. The goal of preventing the overwhelming of medical infrastructure is the most clearly ethical. Next, herd immunity is also justifiable if achieved with proper measures. Near-universal vaccination would be the most difficult to justify based both on a decreasing marginal value of moving beyond herd immunity and the significant level of government intrusion. The goals represent a paradox: the least ambitious but most widely-accepted goal (flattening the curve) warrants the most intrusive government policy, yet the most intrusive policy would go beyond the stated goal and should not be implemented because it is ethically imperative that the state use the least restrictive means to achieve the goal. The most ambitious goal (near-universal vaccination) does not justify universal compulsory vaccination despite being out of reach absent a universal mandate. The support of the public is crucial as a check on government authority and to ensure that the least restrictive means are used to pursue legitimate ends. The public’s input for precisely tailoring vaccination policy to ensure that it is both successful in achieving its goal and ethical will be paramount. What follows is a general framework based on a careful consideration of the issues outlined in the preceding sections of this paper.
1. Most ambitious and most controversial: a near-universal vaccination rate
This goal is ethical insofar as it prevents the most deaths, which is a proper government interest. However, to achieve it, intrusive policies, including any sort of mandate, are not warranted because a) the marginal benefit of moving past herd immunity is low, b) the goal overreaches widely-accepted government action and so puts government too far out of step with citizens, and c) they would undermine public trust and autonomy. In order to achieve this goal, to minimize morbidity and mortality, the state (individual US state or local governments) should restrict its activities to the active promotion of vaccination in the public school system or via “community conversations” and media campaigns. It should take steps to minimize misconceptions about vaccine safety, including describing the robust vaccine monitoring and approval process. The state must be careful to expend a proportionate amount of resources on this effort, not shifting funding away from other important functions. The federal government should restrict its activity to moral leadership and funding these educational initiatives and vaccine development.
2. Moderately ambitious and less controversial: herd immunity
To reduce “community spread” to near zero, it is ethical for the state also to implement well-precedented coercive measures like vaccination requirements for school enrollment and for certain healthcare professionals (granting standard exemptions). During a crisis, it may consider eliminating these exemptions, subsidizing vaccination, and establishing honor-system quarantine requirements for those unvaccinated citizens who travel to other states and return. This is in addition to mask mandates or curfews which reduce spread and, because of their unpopularity, may encourage citizens to choose to be vaccinated to bring the crisis to a speedier end. The federal government should ideally restrict its activity to adding to the vaccination requirements for new or continued military service, regulating industries which receive federal funds, imposing international travel bans, as well as providing moral leadership, funding for state initiatives, and guidelines for regional response uniformity. However, depending on the nature of the crisis, the federal government may assist in regulating interstate travel. Herd immunity is a realistic and ethically justified goal, yet it is closer to the limit of tolerable government authority. Because the public might not accept it, it would be best for social cohesion if it were achieved without a universal compulsory mandate (which would also overshoot the goal).
3. Least ambitious and widely accepted: immunity levels sufficient to prevent the overwhelming of medical infrastructure
Partially because this is the most widely-accepted goal, government should be able to use more intrusive means to achieve it. It balances government interests, autonomy, economic interests, and liberties, and it would add to social cohesion and represent respect for myriad views on what is beneficent. As such, it would warrant the most intrusive policies, including universal compulsory vaccination, yet the government must always use the least restrictive means to achieve an end. If, once it has made vaccines available free of charge (and provided tax credits as an incentive), the state has not met this goal, it is ethical for it to consider implementing more coercive tactics. These range from permitting insurance companies to charge higher premiums for those who refuse vaccination to establishing “immunization cards” (attending to the associated privacy and discrimination concerns) and requiring the presentation of such cards before use of state facilities or services, like public transportation, or for avoiding enforceable quarantine after travel. Presentation of an immunization card should not be a requirement for welfare eligibility, including Medicaid nursing home assistance. If, after some significant period, these tactics fail, the state may consider compulsory vaccination. States should solicit expert and public input for the design of the policy, which may be rolled out from county-to-county based on infection and hospitalization rates. Such a policy should have broad opt-out provisions, at least to begin with, and there should be a mechanism to overturn it by referendum. Imprisonment should not be one of the considered penalties, but, in accordance with Jacobson, paying a fine for failure to become vaccinated should be an option. The federal government should avoid attempting any vaccine mandate of its own, though it may consider withholding highway or other funds from states which refuse to implement even the most basic measures to control the disease’s spread. Once the goal of preventing the overwhelming of the medical infrastructure is met, the compulsory vaccination policy should be reconsidered with an eye to limiting it to school or sector-specific mandates, as these have widespread public acceptance.
CONCLUSION
Universal compulsory vaccination should be part of the conversation on COVID-19 now only insofar as the purpose is informing citizens that it may eventually be a necessity and that pertinent plans must be developed in advance. Despite rising case counts, it is inappropriate for the release of a vaccine to be immediately accompanied by policies requiring members of the general public to receive that vaccine. Every reasonable alternative must be exhausted before such policies are implemented, not only because they touch an issue so central in a free society, the right of individuals to make decisions about what is done to their bodies, but also because of the practical obstacles, including inevitable legal challenges and widespread anger and resentment that could undermine the country’s ability to effectively combat this crisis and the crises that lie ahead.
[1] Corum, Jonathan, Sui-Lee Wee, and Carl Zimmer. 2020. “Coronavirus Vaccine Tracker.” The New York Times, November 13, 2020, sec. Science. https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html.
[2] This paper uses “compulsory vaccination” to apply to vaccination mandated for all in the community with fines as an enforcement tool and not to vaccination of a narrower group as a requirement for participation in school, the workplace, or other public spaces and activities.
[3] Gostin, Lawrence O. 2005. “Jacobson v Massachusetts at 100 Years: Police Power and Civil Liberties in Tension.” American Journal of Public Health 95 (4): 576–81. https://doi.org/10.2105/AJPH.2004.055152.
[4] See Jacobson v. Massachusetts, 197 U.S. 11, 25 S. Ct. 358 (1905).
[5] Gostin, Lawrence O. 2005.
[6] Cole, Jared P, and Kathleen S Swendiman. 2014. “Mandatory Vaccinations: Precedent and Current Laws.” Congressional Research Service. https://fas.org/sgp/crs/misc/RS21414.pdf.
[7] See Zucht v King, 260 U.S. 174, 43 S. Ct. 24 (1922)
[8] Cole, Jared P, and Kathleen S Swendiman. 2014.
[9] Institute of Medicine (US) Forum on Emerging Infections, Stacey L. Knobler, Adel AF Mahmoud, and Leslie A. Pray. 2002. The Model State Emergency Health Powers Act. Biological Threats and Terrorism: Assessing The Science and Response Capabilities: Workshop Summary. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK98412/.
[10] Ibid.
[11] Lederman, Michael, Maxwell Mehlman, and Stuart Youngner. 2020. “Defeat COVID-19 by Requiring Vaccination for All. It’s Not Un-American, It’s Patriotic.” USA Today, August 6, 2020. https://www.usatoday.com/story/opinion/2020/08/06/stop-coronavirus-compulsory-universal-vaccination-column/3289948001/.
[12] Artiga, Samantha, Bradley Corallo, and Olivia Pham. 2020. “Racial Disparities in COVID-19: Key Findings from Available Data and Analysis.” Kaiser Family Foundation. https://www.kff.org/racial-equity-and-health-policy/issue-brief/racial-disparities-covid-19-key-findings-available-data-analysis/.
[13] Gostin, Lawrence O. 2005.
[14] Griswold v. Connecticut, 381 U.S. 479, 85 S. Ct. 1678 (1965)
[15] Cruzan v. Director, Missouri Department of Health, 497 U.S. 261, 280 (1990)
[16] See Mills v Rogers, 457 U.S. 291, 102 S. Ct. 2442 (1982), Washington v. Harper, 494 U.S. 210, 110 S. Ct. 1028 (1990), among others.
[17] Amy Coney Barrett, Neil Gorsuch and Brett Kavanaugh, to name a few. See Schaff, Erin. 2020. “Legal Scholar Warns of Potential Supreme Court Changes.” The Harvard Gazette, October 15, 2020, sec. National & World Affairs. https://news.harvard.edu/gazette/story/2020/10/legal-scholar-warns-of-potential-supreme-court-changes/.
[18] Liptak, Adam. 2020. “Splitting 5 to 4, Supreme Court Backs Religious Challenge to Cuomo’s Virus Shutdown Order.” The New York Times, November 26, 2020. https://www.nytimes.com/2020/11/26/us/supreme-court-coronavirus-religion-new-york.html.
[19] Health Resources & Services Administration. 2020. “National Vaccine Injury Compensation Program.” HRSA.Gov. November 2020. https://www.hrsa.gov/vaccine-compensation/index.html.
[20] Giubilini, Alberto. 2020. “An Argument for Compulsory Vaccination: The Taxation Analogy.” Journal of Applied Philosophy 37 (3): 446–66. https://doi.org/10.1111/japp.12400.
[21] Hoffman, Jan. 2019. “How Anti-Vaccine Sentiment Took Hold in the United States (Published 2019).” The New York Times, September 23, 2019, sec. Health. https://www.nytimes.com/2019/09/23/health/anti-vaccination-movement-us.html.
[22] Reinhart, RJ. 2020. “More Americans Now Willing to Get COVID-19 Vaccine.” Gallup. November 17, 2020. https://news.gallup.com/poll/325208/americans-willing-covid-vaccine.aspxh
[23] Kleinfeld, Rachel. 2020. “Perspective: The U.S. Shows All the Signs of a Country Spiraling toward Political Violence.” Washington Post, September 11, 2020. https://www.washingtonpost.com/outlook/america-political-violence-risk/2020/09/11/be924628-f388-11ea-999c-67ff7bf6a9d2_story.html.
[24] Reiss, Dorit R., and Y. Tony Yang. 2020. “Why a COVID-19 Vaccine Shouldn’t Be Mandatory.” Bill of Health: Examining the Intersection of Health, Law, Bioetechnology, and Bioethics (blog). September 15, 2020. http://blog.petrieflom.law.harvard.edu/2020/09/15/covid19-vaccine-mandate-compulsory/.
[25] Thompson, Stuart A. 2020. “Opinion: How Long Will a Vaccine Really Take?” The New York Times, April 30, 2020, sec. Opinion. https://www.nytimes.com/interactive/2020/04/30/opinion/coronavirus-covid-vaccine.html.
[26] Hermes, Clint. 2020. “Opinion: Covid-19 Vaccines Shouldn’t Get Emergency-Use Authorization.” MIT Technology Review, November 13, 2020. https://www.technologyreview.com/2020/11/13/1012098/covid-19-vaccines-fda-emergency-use-authorization-opinion/. On December 2, 2020, the UK approved Pfizer and BioNTech SE’s vaccine for emergency use. Medicines and Healthcare Products Regulatory Agency, UK, press release, “UK medicines regulator gives approval for first UK COVID-19 vaccine,” December 2, 2020. https://www.gov.uk/government/news/uk-medicines-regulator-gives-approval-for-first-uk-covid-19-vaccine
[27] Aschwanden, Christie. 2020. “The False Promise of Herd Immunity for COVID-19.” Nature 587 (7832): 26–28. https://doi.org/10.1038/d41586-020-02948-4.
[28] Vazquez, Maegan, and Priscilla Alvarez. 2020. “White House Extends National Emergency on the Southern Border.” CNN, February 14, 2020. https://www.cnn.com/2020/02/13/politics/southern-border-national-emergency-continuation/index.html.
[29] WHO. 2009. The WHO Pandemic Phases. Pandemic Influenza Preparedness and Response: A WHO Guidance Document. World Health Organization. https://www.ncbi.nlm.nih.gov/books/NBK143061/.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.

