Humanizing the Physician-Patient Relationship How Gift-Giving and -Receiving Can Be Ethical
Main Article Content
Abstract
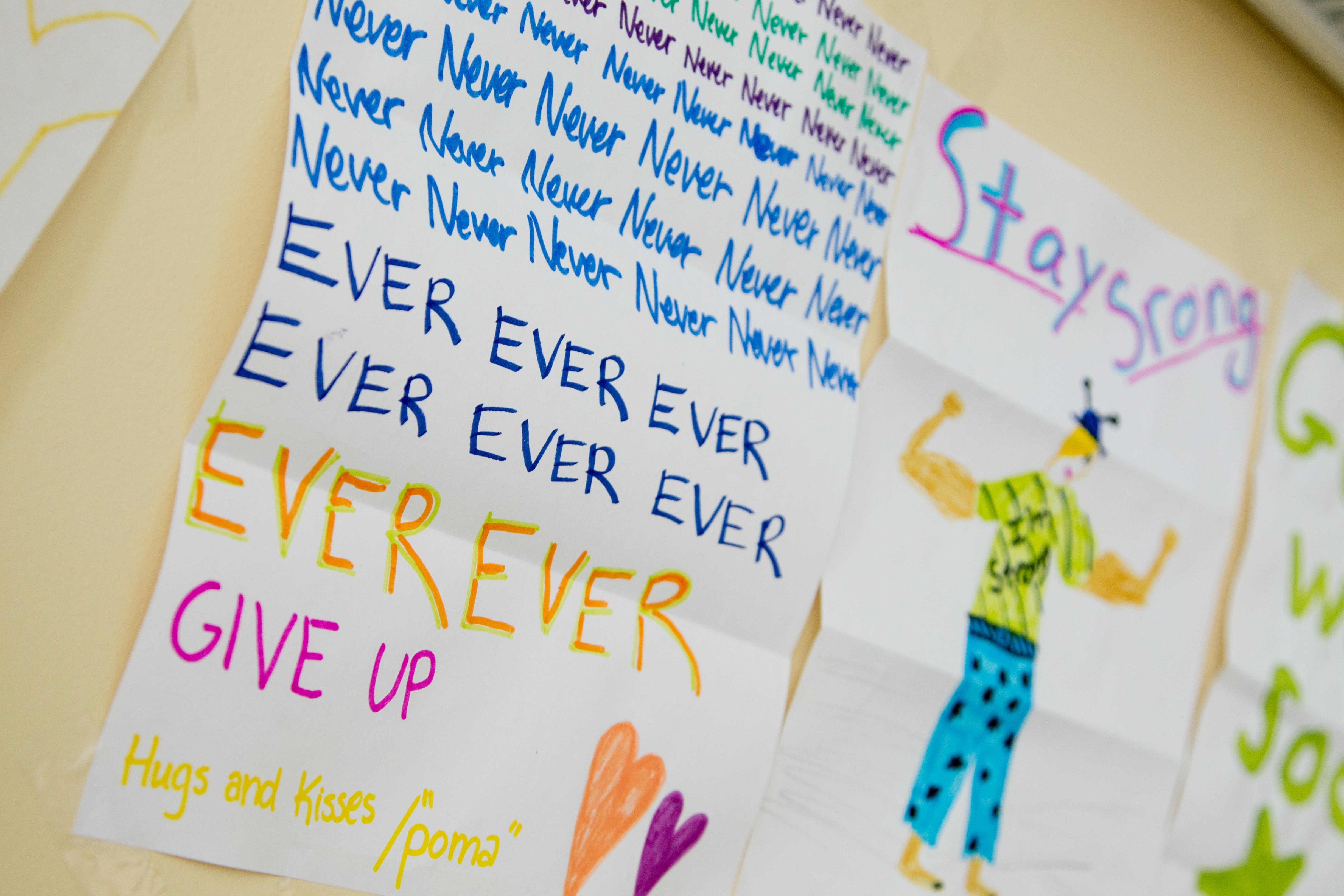
Photo by National Cancer Institute on Unsplash
INTRODUCTION
Gift-giving by patients or their families to physicians has happened since there were patients and physicians, and in many places, it’s still quite common. It’s also potentially problematic, and the why and how of it offer important insight into the physician-patient relationship and human relationships more broadly. Yet ethicists, regulators, and the public have not paid much systematic attention. In the United States, no federal or state legislation directly addresses it. Only in the past two decades did the American Medical Association (AMA) release guidance to physicians about it. That guidance, which permits physicians to accept certain gifts by certain patients under certain circumstances, namely, when it will not influence their medical judgment or cause hardship to the gift-giver, is vague and incomplete – indeed, it’s all of 200 words.[1] Other physician professional organizations have little to add.[2] A few academics and opinion columnists have studied or reflected on the psychology of gift-giving and -receiving and recommended everything from categorical rejection of patient gifts[3] to erring on the side of accepting them, provided they are of modest value, and the motivation behind them can be discerned.[4] However, insufficient attention has been paid to the when and where of those gifts or the significance of clinic-, hospital- or other systems-level ethical safeguards.
ANALYSIS
When deciding whether they will accept a gift from a patient or their family, physicians must balance the possibility that the gift could cloud medical judgment, lead to favoritism, exploitation, and slippery slopes, or pressure other patients to give, and perhaps even debase the meaning of medical treatment, against the prospect that gift-giving could increase patient trust and satisfaction, as well as empower patients and respect their autonomy and culture.[5] Performing this harm-benefit calculation case by case is challenging and time-consuming. Unsurprisingly, many physicians opt simply to tell would-be gift-giving patients that they appreciate the sentiment, but, as a rule, they accept no gifts. I submit many physicians do this also because they are unaware of how meaningful giving a gift can be for patients or anyone in a disadvantaged position with respect to the gift recipient. They may also not know that there are simple accountability mechanisms they can institute that may prevent many of the possible adverse consequences of gift-giving and -receiving in the context of the physician-patient or physician-patient-family relationship. Unfortunately, many instances in which accepting a gift would have led to net benefit are foregone.
It is my belief a consensus could quickly be formed about which types of gifts would clearly be wrong to accept. Few would defend the physician who agrees to use a patient’s villa in the Bahamas or welcomes expensive jewelry or lewd photos. The timing and intent of a gift also matter. Few would forgive the physician who accepted even a modestly valuable voucher to eat at a patient’s restaurant while their eligibility for transplant was being debated or after they had run out of opioid painkillers and were denied a prescription renewal. On the other hand, I doubt even Charles Weijer or the College of Physicians and Surgeons of Prince Edward Island, which views accepting gifts from patients as “boundary crossing,”[6] would demand an orthopedic surgeon turn down the happy picture a pediatric patient drew after recovering from a hip injury and resuming sports. They are also unlikely to criticize an oncology team that graciously receives a fruitcake baked by the sister of an elderly cancer patient after the decision was made and agreed to, around Christmastime, not to initiate another round of chemotherapy.
These unlikely refusals may be because rejecting those gifts, all things considered, would seem cruel. But it might also be because there is disagreement about what constitutes a gift: whether it must be a tangible object (are heartfelt thank-yous and hugs not also “gifts”?) or whether it must be something that requires the physician actively do something, e.g., get on a plane. These disagreements about definitions may also partially underlie disagreements about practice. Suppose a patient in a sparsely populated, heavily wooded part of Maine takes it upon himself to offer a sack of apples from his orchard to his internist, who regularly waives fees for those who cannot pay them or will make a house call at any time of the night. In that case, the internist may not consider the apples a gift. He may not think of them as payment or re-payment either. They may exist in some in-between category, much like the knitted slippers brought in by a patient in whose culture “thank you” is seldom said.
But clearly, some things are widely perceived as gifts or to have substantial gift-like character. Should they, at least, be rejected? I don’t think so. The act of gift-giving and -receiving can be a sort of ritual and gradually lead to trust and closeness.[7] Perhaps a shy patient whose wife previously sent chocolates to his physician around Christmastime will come to see the physician as a part of his extended family. Perhaps he needs to do so to feel comfortable talking about his erectile dysfunction. Gifts can be expressions of caring.[8] Perhaps an elderly Texan patient imagines her younger physician, whom she has known for thirty years and often sees at the grocery store, as her son and asks to prepare a homecoming mum (traditionally a chrysanthemum flower corsage) for his children’s school dance. Perhaps doing so will give her purpose, make her feel useful, as all her own children have moved away. Giving gifts may also provide patients with a sense of control and help them feel as if less of a power imbalance exists between them and their physician. Perhaps a young judge, who is not used to not being in control, and was previously misdiagnosed with rheumatoid arthritis, is now struggling to come to terms with his Lupus. Perhaps giving the physician who made the correct diagnosis a moderately-priced bottle of scotch restores his confidence or sense of pride.
Gifts are also undoubtedly important to the recipient. When medical providers receive a gift, they may interpret it as a sign that they are valued. While it would be wrong to practice medicine to receive gifts or expect them, there are times, like when ERs and ICUs are overwhelmed because of a viral pandemic,[9] which threatens the will to continue working, and most anything (within reason) that bolsters resolve can be considered good. There is also no obvious distinction between the satisfaction physicians normally receive on seeing their patients recover or being thanked or smiled at and what they feel when they receive a small or “token” gift, like a plate of homemade cookies.
The point is that the physician-patient relationship is a human one. Many advocate it should be personal, that physicians should be emotionally invested in their patients, care about and have compassion for them in ways that professional oaths do not fully capture.[10] This dynamic is particularly important in primary care or when the physician-patient relationship continues for long periods. According to one Israeli study, many patients even wish for a relationship with their physician akin to friendship. Those who felt they had such a relationship were more satisfied with their care than those who believed the relationship was business-like.[11] The precedent for this “friendship between unequals” goes back at least to the time of Erasmus, some five hundred years ago.[12] There may be good reasons for physicians to draw the line before friendship, but if accepting certain gifts builds intimacy, and that intimacy does not cross over into an inappropriate relationship, e.g., a sexual or romantic relationship, and if it has the chance to improve healthcare outcomes through improved mood or early disclosure of problems, I think it should be done. Physicians have a prima facie duty to do good for their patients.[13] Most physicians want to do good for their patients and respect their traditions and preferences. I suspect that accepting the gifts from the patients in the examples above would do a lot of good, or at least that rejecting them could do significant harm, including making them or their families feel estranged from the medical community, impeding future care.
Physicians might be more comfortable accepting gifts if receiving gifts would not subject them to scrutiny or penalty. They also may feel better if they knew that receiving gifts would not harm their patients and that rejecting gifts might. They should document all gifts they receive.[14] This will enable them to detect if gifts from a particular patient are increasing in frequency or lavishness or changing markedly in character, which could warrant attention. I maintain this “Gift Log” should be maintained in common with everyone at the clinic or in the relevant hospital department and potentially made available to hospital administration for audit. Investigation might be necessary if a gift is given (and accepted) with no explicable context, e.g., not near holiday season or after a treatment milestone is achieved. When possible, gifts should be shared communally, such as placing fruit baskets or chocolates in the staff room. Other gifts, like artwork, can be displayed on the walls.
Others should be encouraged to hold physicians accountable if they feel patients who have given gifts receive preferential treatment, including something as seemingly small as priority for appointment bookings. Appearances matter and even the appearance of impropriety can affect the public’s trust in medicine. The culture of medicine has already changed such that nurses now reproach physicians they feel violate the standard of care,[15] and this would be an extension of that trend. Depending on the set-up of the practice, a staff member can be designated for receiving gifts and politely declining those that ought to be declined. Staff members should tell patients, who give gifts in full view of other patients, that they cannot do so in the future. Physicians can politely rebuff patients who wish to give inappropriate gifts, or gifts at inappropriate times and suggest they donate to charity instead. Medical practices and hospitals should develop a gift policy in consultation with staff and patients to avoid needlessly rejecting gifts that benefit both doctor and patient and to avoid pressuring patients into giving gifts. The policy should be flexible to account for the crucial human element in any provider-patient relationship and the cultural nuances of any practice setting. Psychiatrists, who work with particularly vulnerable patients, may need to be more vigilant when accepting gifts.[16]
CONCLUSION
Though we tend to think health innovation occurs in urban medical centers and spreads outward, there may be something big-city physicians can learn from their rural colleagues about personalized patient-physician relationships. The value of gifts is only one example. Normalizing the acceptance of patient gifts in appropriate restricted circumstances has the added benefit of shining a spotlight on the acceptance of patient gifts in dubious ones. By bringing an already fairly common practice into the open and talking about it, we can create policies that respect patients as persons, prevent abuse, and deconstruct the stereotype of the austere and detached physician. While there is no reason to think that gift-giving would get out of control if appropriate safeguards are put in place, the medical community can always re-evaluate after a period, or an individual medical practice can re-evaluate based on the circumstances of their practice environment. Gift-giving, especially when gifts are of small monetary value, should be recognized as a culturally appropriate gesture with meaning far beyond that monetary value. It is best governed by reasonable gift-giving policies, not banned altogether.
-
[1] Council on Ethical and Judicial Affairs. “Ethics of Patient-Physician Relationships.” In AMA Code of Medical Ethics, 11. Chicago: American Medical Association, 2021. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/code-of-medical-ethics-chapter-1.pdf.
[2] Sulmasy, Lois Snyder, and Thomas A. Bledsoe. “American College of Physicians Ethics Manual.” Annals of Internal Medicine 170, no. 2_Supplement (January 15, 2019): S1–32. https://doi.org/10.7326/M18-2160; Committee on Bioethics. “Pediatrician-Family-Patient Relationships: Managing the Boundaries.” Pediatrics 124, no. 6 (December 1, 2009): 1685–88. https://doi.org/10.1542/peds.2009-2147.
[3] Weijer, Charles. “No: Gifts Debase the True Value of Care.” Western Journal of Medicine 175, no. 2 (August 2001): 77.
[4] Lyckholm, Laurie J. “Should Physicians Accept Gifts From Patients?” JAMA 280, no. 22 (December 9, 1998): 1944–46. https://doi.org/10.1001/jama.280.22.1944; Spence, Sean A. “Patients Bearing Gifts: Are There Strings Attached?” BMJ 331, no. 7531 (December 22, 2005): 1527–29. https://doi.org/10.1136/bmj.331.7531.1527; Gaufberg, Elizabeth. “Should Physicians Accept Gifts from Patients?” American Family Physician 76, no. 3 (August 1, 2007): 437; Caddell, Andrew, and Lara Hazelton. “Accepting Gifts from Patients.” Canadian Family Physician 59, no. 12 (December 2013): 1259–60.
[5] See above commentators and Drew, Jennifer, John D. Stoeckle, and J. Andrew Billings. “Tips, Status and Sacrifice: Gift Giving in the Doctor-Patient Relationship.” Social Science & Medicine 17, no. 7 (January 1, 1983): 399–404. https://doi.org/10.1016/0277-9536(83)90343-X.
[6] College of Physicians and Surgeons of Prince Edward Island. “Respecting Boundaries.” Accessed April 4, 2021. https://cpspei.ca/respecting-boundaries/.
[7] The Atlantic’s Marketing Team. “What Gifting Rituals from Around the Globe Reveal About Human Nature.” The Atlantic, 2018. https://www.theatlantic.com/sponsored/hennessy-2018/what-gifting-rituals-around-globe-reveal-about-human-nature/2044/.
[8] Parker-Pope, Tara. “A Gift That Gives Right Back? The Giving Itself.” The New York Times, December 11, 2007, sec. Health. https://www.nytimes.com/2007/12/11/health/11well.html.
[9] Harlan, Chico, and Stefano Pitrelli. “As Coronavirus Cases Grow, Hospitals in Northern Italy Are Running out of Beds.” Washington Post. Accessed April 4, 2021. https://www.washingtonpost.com/world/europe/italy-coronavirus-patients-lombardy-hospitals/2020/03/12/36041dc6-63ce-11ea-8a8e-5c5336b32760_story.html.
[10] Frankel, Richard M. “Emotion and the Physician-Patient Relationship.” Motivation and Emotion 19, no. 3 (September 1, 1995): 163–73. https://doi.org/10.1007/BF02250509.
[11] Magnezi, Racheli, Lisa Carroll Bergman, and Sara Urowitz. “Would Your Patient Prefer to Be Considered Your Friend? Patient Preferences in Physician Relationships.” Health Education & Behavior 42, no. 2 (April 1, 2015): 210–19. https://doi.org/10.1177/1090198114547814.
[12] Albury, W. R., and G. M. Weisz. “The Medical Ethics of Erasmus and the Physician-Patient Relationship.” Medical Humanities 27, no. 1 (June 2001): 35–41. https://doi.org/10.1136/mh.27.1.35.
[13] Beauchamp, Tom L., and James F. Childress. Principles of Biomedical Ethics. 7th edition. New York: Oxford University Press, 2012.
[14] Caddell and Hazelton, 2013.
[15] See, e.g. Peplau, Hildegard E. “A Glance Back in Time: Nurse-Doctor Relationships.” Nursing Forum 34, no. 3 (1999): 31–35. https://doi.org/10.1111/j.1744-6198.1999.tb00991.x and Ahmad, Ahmir. “The Doctor-Nurse Relationship: Time for Change?” British Journal of Hospital Medicine (2005), September 27, 2013. https://doi.org/10.12968/hmed.2009.70.Sup4.41642.
[16] Hundert, Edward M. “Looking a Gift Horse in the Mouth: The Ethics of Gift-Giving in Psychiatry.” Harvard Review of Psychiatry 6, no. 2 (January 1, 1998): 114–17. https://doi.org/10.3109/10673229809000319.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.