Repurposing the Ladder Liberty, Choice, and Autonomy as Applied to India’s COVID-19 Vaccination Drive
Main Article Content
Abstract
Photo by Mufid Majnun on Unsplash
INTRODUCTION
In 2007, the Nuffield Council of Bioethics introduced the “Intervention ladder” as a guiding framework[1] to evaluate the impact on individual liberty of various public health measures. One criticism of the ladder is that it reflects a narrow view of liberty, yet other researchers adapted the intervention ladder to incorporate a more autonomy-based view. Recently, academics and public health officials have used intervention ladders as guides in framing policies, particularly COVID-19 pandemic policies.[2] Analyzing the Indian COVID-19 vaccination drive under these two ladders can illuminate the concepts of liberty underlying those ladders and help determine the best framework on a philosophical basis.
ANALYSIS
l. Case Study: The Indian COVID-19 Vaccination Drive
On January 16, 2021, India attempted a public vaccination drive.[3] The drug regulatory body Central Drugs Standards Control Organization (CDSCO) approved two vaccines, Covishield and Covaxin, for emergency use.[4] The approval was granted despite a clear lack of phase 3 clinical trial data for both of these vaccines.[5] Covishield, produced by the Serum Institute of India, is the Indian variant of the Astra-Zeneca vaccine that has shown an average efficiency of 70.4 percent after trials in the UK.[6] Covaxin, manufactured by Bharat Biotech in collaboration with the Indian Council of Medical Research (ICMR) National Institute of Virology, was developed and manufactured in India. [7]
Covishield relied on the safety and efficacy data from large trials conducted in Brazil, South Africa, and the UK with 24,000 participants and a small cohort for the Indian study. Covaxin was given approval based only on phase-1 trial data.[8] An article published in The Lancet called for further efficacy data from the Covaxin study.[9] The officials associated with Bharat Biotech, as well as the Indian Council of Medical Research, maintained that fast production of the vaccine does not indicate a compromise in safety, even though they had little data to produce.[10] However, transparency is key to vaccination policy, which requires public participation.
The media reported that the Covaxin clinical trials compromised research integrity by providing a monetary incentive of around 7 euros, to research subjects. People’s University, a private medical college, and hospital, recruited survivors of the Bhopal Gas tragedy for the Covaxin study. The participants were told that they were being provided a vaccine against COVID-19 without clarifying that data was being collected for their clinical study. There was no record of informed consent from these participants for the Covaxin study.[11] The media reported the death of a 42-year-old individual who received his first dose on December 23, 2020.[12] Although it was reported that the cause of death was not linked to the vaccine, the death added to vaccine hesitancy. The vaccines were provided for free to the frontline healthcare workers with no choice on which vaccine the recipients would receive.[13] Similarly, in the US, some people do not have a choice between Pfizer or Moderna. In the UK and the US, data from phase 3 trials are known with a periodic follow-up after the administration of the second dose.[14] The WHO developed a tracking system for COVID-19 vaccine recipients which was updated on March 19, 2021, to reflect the results of Covaxin phase 3 trials.[15]
India eliminated choice although the two vaccines approved for emergency use did not have the depth of research that those used elsewhere had. The intervention ladder, discussed below, which uses proportionality and the harm principle to justify the lack of choice between the vaccines in the UK and the US, should not be applied to India’s vaccination policy.
ll. The Nuffield Intervention Ladder
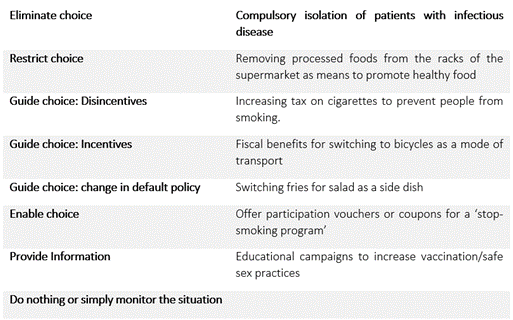
The foundational principle underlying the Nuffield Intervention Ladder is Mill’s conception of individual liberty from the prominent work, On Liberty.[16] However, the Council recognizes that the intervention ladder is conceived on a broader interpretation of Mill’s liberty, using the principle of proportionality as a tool for justification i.e., the desired effect from the intervention is proportional to the loss incurred in liberty.[17] As shown in Table 1, an ideal intervention that is least infringing would then be no intervention at all. An intervention that would be more difficult to justify would be one that significantly restricts individual liberty. Intuitively, eliminating occupies the topmost rung on the ladder. The metaphor of the ladder suggests that as one climbs up the rungs of the ladder, stronger justifications would be required.
Table 1: Examples of interventions at each level of the intervention ladder adapted and improvised from the Nuffield Council of Bioethics Report, 2007.
A voluntary vaccination policy is one public health intervention that is acceptable and justifiable in terms of the principle of proportionality as well as Mill’s Harm Principle, with emphasis on diminishing individual liberties when actions might result in harm to others.[18] Although a vaccination policy in the context of a global pandemic seems justifiable through the lens of the intervention ladder, the Indian modus operandi is unique because of inherent problems with the original conception of the intervention ladder. By pausing to elaborate and reflect on the Indian context as a case study, we can demonstrate that individual liberty should not be the sole variable in framing justifiability.
lll. Critiquing the Nuffield Intervention Ladder & Adding a Precautionary Approach
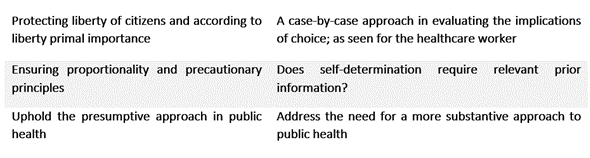
In his paper, ‘Snakes and Ladders: State Interventions and the Place of Liberty in Public Health Policy’, Angus Dawson criticizes the intervention ladder’s focus on individual liberty,.[19] and its inability to account for the different treatment of incentives and disincentives and the role of information. Public health institutions require public participation to restrict the infectious spread of COVID-19. The lack of transparency and minimal information surrounding the vaccines have been a major hurdle in increasing public participation. It is contradictory to think that the public does not require information about interventions and have the ability of self-determination to guide them, when in fact self-determination presupposes possession of relevant information.
A voluntary vaccination policy can be seen as sitting on either the lowest rung (providing information) or the rung of enabling choice, as a vaccination campaign does both. However, in India, the precautionary principle should also be applied as providing the choice should not permit ‘harm’. The precautionary principle holds that anything that poses a risk to human health or the environment should be avoided or accompanied by precautionary measures. In India, because the clinical trials were smaller and there is less proof of safety and efficacy, a vaccination requirement, or a public health campaign to encourage vaccination violates the principle. The proportionality principle governing the intervention ladder only requires that the benefits of the intervention justify the restrictions on liberty. The intervention ladder should prevent requiring healthcare worker vaccination without a choice of vaccine because a free choice requires transparency and more information than is available from the small early-stage clinical trials. Actions surrounding the vaccines in India do not reflect proper precaution or a proportionate and thus acceptable restriction on liberty. If there is no ability to choose between the two possible vaccines, then they should not be mandatory for healthcare workers.
The Indian government and its officials have urged healthcare worker compliance by invoking the seriousness of the pandemic and the alarming rates of mortality rather than providing transparent data pursuant to the regulatory mechanisms of the vaccine clinical trial. For a healthcare worker, the duty to provide service and a stronger obligation to do so in the time of a pandemic already imposes certain restrictions on their liberty. The lack of choice in opting for a preferred vaccine puts it on a higher rung on the intervention ladder and thus requires stronger justifications. This case study reveals how the same public health intervention falls on different rungs of the intervention ladder depending on the target group in consideration. Or to put this simply, choice is contextual.
Table 2: The ethical values at stake when it comes to “choice”
lV. An Autonomy-Based Intervention Ladder
Liberty and autonomy differ slightly: liberty revolves around the constraints on the ability to act, whereas autonomy stresses on the independence and the authenticity of the willingness to act.[20] It is thus possible for an individual to be autonomous but unfree, as can be seen from the inability to opt for a preferred vaccine.[21] Figure 1 shows an adapted schematic of an autonomy-based intervention ladder as proposed by Griffiths et al.
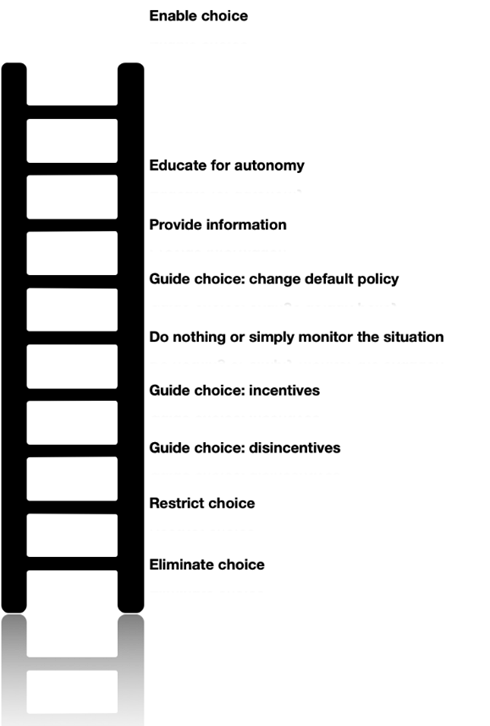
Figure 1: An adapted schematic of the autonomy-based intervention ladder proposed by Griffiths, P.E and West, C.
In comparing the original intervention ladder with their proposal, we see that the autonomy-based model allows for a negative scale in terms of its effects on autonomy. Thus, on this ladder, actions can be autonomy-enhancing or autonomy-diminishing. Such a model challenges the one-directional view of the ladder and rearranges interventions on a scale that ranges from negative to positive. A few interventions that were shown to have restrictive effects on liberty now have reinforcing effects when viewed through the lens of autonomy. Thus, providing information and educating can be seen as positive reinforcements for autonomous choice rather than infringing on individual liberty.
The autonomy-based intervention ladder requires the State to implement interventions and design policies in a manner that reinforces autonomy. Information and education allow individuals to be free and equal participants in public health discourses.
As seen in the original intervention ladder restricting choice, as well as eliminating it, still fall in the negative, autonomy-infringing side of the ladder. Thus, requiring stronger justifications for their implementation. The only difference between the two is the manner in which the new model ensures the availability of a choice when the precautionary, as well as the proportionality principle, have not been met to a sufficient extent. Ensuring choice and exercising it becomes much more relevant in making people autonomous. The frontline worker thus can opt for a vaccine they prefer. Thereby, helping them navigate the moral conundrum of opting to get vaccinated, easing their moral burden. It also places strict vigilance over regulatory mechanisms that are involved in clinical trials since the burden of proof now involves providing information as a clear operational motive. This ameliorates public tendencies of hesitancy can be alleviated in this respect. An autonomy-based intervention ladder is not in conflict with Mill’s conception of liberty since Mill himself does not automatically assume a cost to liberty when the State seems to employ public education campaigns to inform the public.[22]
CONCLUSION
The original intervention ladder was conceived to remedy the hurdles that a traditional liberal landscape brings in implementing a public health intervention and to protect individual liberties. The intervention ladder assumes an inverse relationship between public health and freedom. Rethinking the intervention ladder from a different perspective allows a proper role of the dissemination of information, recognizing that consent relies on information. An autonomy ladder acts as a starting point for rethinking public health and how it can foster autonomy as well as impede it. By focusing on autonomy, the benefits that can be gained from educational and informational campaigns are viewed as reinforcing autonomy. Autonomy is vital to liberty. COVID-19 has brought a unique set of ethical issues that have questioned conventionally accepted frameworks and calls for a substantive, alternative approach to public health ethics.
[1] Nuffield Council on Bioethics, “Public Health: Ethical Issues.” Nuffieldbioethics.org, Nov 13, 2007. www.nuffieldbioethics.org/publications/public-health. Accessed 9 May 2021.
[2] Giubilini A, The Ethics of Vaccination [Internet]. Cham (CH): Palgrave Pivot; 2019. Chapter 3, “Vaccination Policies and the Principle of Least Restrictive Alternative: An Intervention Ladder.” 2018 Dec 29, 2018. www.ncbi.nlm.nih.gov/books/NBK538385/.
[3] Dash, Sachinta. “India Begins Its COVID-19 Vaccination Drive — Here’s a Look at How the World’s Largest Vaccine Rollout Is Set to Take Place.” Business Insider India, January 16, 2021, www.businessinsider.in/india/news/india-will-begin-its-covid-19-vaccination-drive-tomorrow-heres-everything-you-need-to-know/articleshow/80281740.cms. Accessed 9 May 2021.
[4] Special Correspondent, “Coronavirus | India Approves COVID-19 Vaccines Covishield and Covaxin for Emergency Use,” The Hindu, January 3, 2021, www.thehindu.com/news/national/drug-controller-general-approves-covishield-and-covaxin-in-india-for-emergency-use/article33485539.ece. Accessed 9 May 2021.
[5] Thiagarajan, Kamala, “Covid-19: India Is at Centre of Global Vaccine Manufacturing, but Opacity Threatens Public Trust.” BMJ, January 28, 2021. www.bmj.com/content/372/bmj.n196, 10.1136/bmj.n196.
[6] Thiagarajan, Kamala.
[7] Bharat Biotech, “COVAXIN - India’s First Indigenous Covid-19 Vaccine | Bharat Biotech.” www.bharatbiotech.com/covaxin.html.
[8] Prasad, R. “Coronavirus | Vaccine Dilemma — to Take or Not to Take Covaxin.” The Hindu, January 15, 2021, www.thehindu.com/sci-tech/health/vaccine-dilemma-to-take-or-not-to-take-covaxin/article33577223.ece.
[9] Ella, Raches, et al. “Safety and Immunogenicity of an Inactivated SARS-CoV-2 Vaccine, BBV152: A Double-Blind, Randomised, Phase 1 Trial.” The Lancet Infectious Diseases, vol. 21, no. 5, January 21, 2021, pp. 637–646, www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30942-7/fulltext, 10.1016/S1473-3099(20)30942-7.
[10] Thiagarajan, Kamala.
[11] Thiagarajan, Kamala.
[12] Nichenametla, Prasad. “Bhopal Volunteer’s Death Unrelated to Covaxin, Says Bharat Biotech.” Deccan Herald, 9 Jan. 2021, www.deccanherald.com/national/bhopal-volunteers-death-unrelated-to-covaxin-says-bharat-biotech-937199.html.
[13] Thiagarajan, Kamala.
[14] Thiagarajan, Kamala.
[15] World Health Organization, “Draft Landscape of COVID-19 Candidate Vaccines.” www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines. Accessed 9 May 2021.
[16] John Stuart Mill. On Liberty. 1859. S.L., Arcturus Publishing Ltd, 1859.
[17] Nuffield. “Public Health: Ethical Issues.”
[18] John Stuart Mill. On Liberty. p 13.
[19] Dawson, Angus J. “Snakes and Ladders: State Interventions and the Place of Liberty in Public Health Policy.” Journal of Medical Ethics, vol. 42, no. 8, May 23, 2016, pp. 510–513, 10.1136/medethics-2016-103502.
[20] Griffiths, P.E., and C. West. “A Balanced Intervention Ladder: Promoting Autonomy through Public Health Action.” Public Health, vol. 129, no. 8, August 2015, pp. 1092–1098, pubmed.ncbi.nlm.nih.gov/26330372/, 10.1016/j.puhe.2015.08.007
[21] Thaler, Richard H, and Cass R Sunstein. Nudge: Improving Decisions about Health, Wealth, and Happiness. London, Penguin Books, 2008.
[22] Griffiths, P.E., and C. West.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.

