Why We Don’t Need a MERS Vaccine
Main Article Content
Abstract
On the heels of the Ebola outbreak, the globe is confronting another potential pandemic – the Middle Eastern respiratory syndrome (MERS) virus. With reported cases now reaching at least 26 countries[i] and the death total climbing towards 500,[ii] MERS has surfaced to international attention since its initial outbreak in Saudi Arabia in 2012. In particular, the global scale of this infectious disease has moved the scientific community to antagonize big pharmaceutical companies for not developing a vaccine.[iii]
However, is the attention on the need for a vaccine truly warranted? Below are three critiques for why a MERS vaccine is not necessary.
- According to the UN, MERS is not a global threat.[iv] MERS transmission is substantially lower than the Severe Acute Respiratory Virus (SARS), a virus in the same family as MERS that claimed over 800 lives globally in 2003.[v] Despite being about four times more fatal than SARS, MERS is 90 times less transmissive.[vi] In addition, according to officials in Saudi Arabia and South Korea, where the outbreak is most prevalent, the death rate from MERS is slowing.[vii],[viii] Also, there is no evidence that the MERS virus is mutating into more dangerous forms.
- The global outbreak is the result of ill-prepared public health systems. About half of the cases in South Korea have been linked back to a single hospital, where a delayed diagnosis resulted in 900 people coming into contact with an infected individual.[ix]Additionally, the deadly impact of MERS in Saudi Arabia, which claims 30% of deaths worldwide, is largely due to the Saudi Kingdom’s resistance to accept foreign assistance.[x] Experts believe that the spread of MERS both within Saudi Arabia and globally could have been mitigated, and even stopped entirely, had Saudi authorities been willing to cooperate with public health entities, such as the World Health Organization (WHO). Given this context, the call for a vaccine may actually be undeserved, and rather the global outbreak unveils systemic failings in the international preparedness for infectious disease outbreaks.
- Vaccine development and deployment present substantial challenges. From research and discovery to product registration, it takes about US$200-900 million[xi] and 10 years[xii] to deliver a final, licensed vaccine. Also, only about 6% of vaccines will successfully progress through preclinical testing and enter the market.[xiii] In addition, having a ready vaccine does not guarantee that all individuals will have access to it. Failed vaccine campaigns are all too prevalent.[xiv] These issues make clear that vaccines cannot replace, only augment, public health systems.
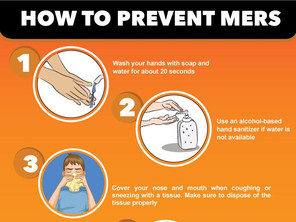
Vaccines are incredible public health tools for combating infectious disease. However, they are not a silver bullet. Public health preparedness for infectious disease requires a comprehensive strategy for prevention and mitigation. According to the WHO’s International Health Regulations Emergency Committee, the MERS outbreak in South Korea is a “wakeup call.”[xv] The main factors contributed to the rapid spread of the infection included a lack of awareness among health workers and the general public about MERS, poor prevention and control measures, crowded emergency rooms, infected patients seeking care at multiple hospitals, and the custom of allowing many visitors to be at the bedside of patients. A vaccine cannot fix these problems.
In response to the outcry from the scientific community that “there’s no excuse for our lack of a MERS vaccine,”[xvi] I argue that their emphasis is misdirected. I believe there are two virtues that offer valuable insight into the issue. The first is responsibility. What MERS has highlighted is that there is no excuse for ill-prepared, unequipped, and underfunded public health systems. While pharmaceutical companies may have a moral obligation to develop life-saving medicines, the burden of responsibility falls on national and international officials to protect its citizens. In this case, pharmaceutical companies should not be held responsible, but the public health systems and officials that have failed their citizens.
The second is prudence. While vaccines are often the most cost-effective intervention to combat infectious disease, not all infectious diseases warrant a vaccine. The evidence supporting immunization is skewed by vaccines that have brought seven major diseases under control – smallpox, diphtheria, tetanus, yellow fever, whooping cough, polio, and measles.[xvii] The smallpox vaccine alone prevents five million deaths a year. With fewer than 500 deaths globally over 3 years, MERS is simply not in the same category. Currently, the big three diseases – HIV/AIDS, malaria, and tuberculosis – claim millions of lives annually and neglected tropical diseases affect more than a billion individuals. The limited resources available for global public health investment should be focused on those causes. Additionally, it is estimated that less than one percent of microbes have been identified by scientists.[xviii] It will not be feasible to develop a vaccine for each and every deadly pathogen that arises in the future.
I believe the 2002-2003 SARS outbreak provides an optimistic outlook to end on. In as fast as it gripped the world, SARS was virtually eradicated as a threat and without a vaccine.[xix] If those responsible take ownership over their mistakes and the international community prudently invests in protecting its citizens from infectious diseases, it may be possible for MERS to have the same fate.
References:
[i] http://www.who.int/csr/disease/coronavirus_infections/faq/en/
[ii] http://www.cnn.com/2015/06/25/asia/south-korea-mers-toll/
[iii] http://www.reuters.com/article/2015/06/15/health-mers-vaccine-idUSL5N0YY2GG20150615
[iv] http://www.usnews.com/news/world/articles/2015/06/17/un-spread-of-mers-in-south-korea-isnt-global-emergency
[v] http://www.who.int/csr/sars/country/2003_07_11/en/
[vi] http://www.healio.com/infectious-disease/emerging-diseases/news/print/infectious-disease-news/%7B422866a7-0445-49b3-ac14-54b39bebbba6%7D/mers-vs-sars-compare-and-contrast
[vii] http://english.alarabiya.net/en/News/middle-east/2015/03/23/MERS-infection-death-rates-slowing-down-says-Saudi-govt.html
[viii] http://www.ndtv.com/world-news/rate-of-mers-infections-in-south-korea-slows-with-1-new-case-773136
[ix] http://www.reuters.com/article/2015/06/23/us-health-mers-southkorea-outbreak-idUSKBN0P300920150623
[x] http://www.reuters.com/article/2014/05/22/us-saudi-mers-specialreport-idUSBREA4L03D20140522
[xi] http://www.ncbi.nlm.nih.gov/pubmed/12477303
[xii] http://www.ncbi.nlm.nih.gov/pubmed/21722688
[xiii] http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3603987/
[xiv] http://blogs.plos.org/speakingofmedicine/2011/09/12/failed-vaccine-campaigns-are-a-global-issue/
[xv] http://www.who.int/mediacentre/news/statements/2015/ihr-ec-mers/en/
[xvi] http://www.huffingtonpost.com/2015/06/15/why-no-mers-vaccine-lack_n_7584380.html
[xvii] http://www.unicef.org/pon96/hevaccin.htm
[xviii] http://bioscience.oxfordjournals.org/content/54/12/1064.full
[xix] http://www.huffingtonpost.ca/2013/03/11/sars-2013_n_2854568.html