Drug Policy Places New Pressures on Hospice
Main Article Content
Abstract
The Policy
After outcry over a new rule intended to help avoid duplicate payments for medications of hospice beneficiaries, the Centers for Medicare and Medicaid Services met June 25th with representatives of thirty hospice organizations, who argue they now face financial burdens that are not theirs to bear.
The rule took effect in May, requiring a prior authorization process for hospices and Part D providers to determine responsibility of drug coverage. Hospices must now cover medications unrelated to the hospice diagnosis. Previously, Part D providers covered drugs for hospice patients’ unrelated conditions,while hospices covered only those drugs for symptom management.
The CMS guidance, entitled “Part D Payment for Drugs for Beneficiaries Enrolled in Hospice,” resulted from a recommendation of the Office of the Inspector General. In 2012, the OIG exercised oversight to examine Medicare hospice patients whose drugs were sometimes paid for by Part D rather than by the hospice. Errors occurred in some instances, and Part D plans had been used to pay for drugs that fell under the responsibility of hospices.
More than 40 organizations- including the American Medical Association, the American Society of Clinical Oncology, and the American Geriatrics Society- issued a letter to CMS Administrator Marilyn Tavenner on June 23rd, calling for the suspension of this policy. Signatories expressed concerns that the rule places beneficiaries at the center of potential disagreements between hospice providers and Part D plans– “requiring dying patients to navigate payer disputes.” It outlines a need for greater clarity in a policy “subject to differing interpretation, and already creating barriers for dying patients who are trying to access necessary medications.”
The signatories cite reports of patients already paying out-of-pocket for medications, going without medications they need, or revoking the hospice benefit in order to access medicine through Part D.
Though a spokesperson for the National Hospice and Palliative Care Organization says members are “pleased” CMS heard concerns, there was “no indication” that any amendments to this new guidance would be made.
Its Implications
While CMS quite validly seeks to ensure the appropriate entities pay for appropriate medications, there exists equally valid concern among providers that such a policy could impact access to quality end-of-life care. The impact is currently being felt financially and administratively, and the implications raise ethical concerns about the future of hospice access.
Financial: The operational strain the CMS guidance places on hospices is tremendous, as providers are responsible for coverage of medical care, social services, nursing visits, chaplaincy, and other support in patient homes, for an average Medicare reimbursement of 160 dollars daily. Added bureaucracy and costs are not pressures hospices are structured to absorb, as typical margins are extraordinarily tight.

Angels Grace Hospice, which serves roughly 45 patients daily in Chicago’s southwest suburbs, has experienced a 30 percent increase in drug costs during the past month. It is covering all drugs while the situation is assessed; a policy Chief Financial Officer Greg Zrazik calls a “fairly liberal, compassionate approach.”
Since only a matter of weeks has passed since its effective date, an accurate financial strain has yet to be measured. “When you have a certain model in anticipation of cost structure and have the situation change, it requires some shifting and adapting and being creative,” Zrazik says. “You’re going to see a more aggressive policy with new patients to assess all medications they are on and look to aggressively discontinue as many drugs as possible when they come on hospice.”
Such an uptick in drug costs threatens the existence of small to mid-sized hospices throughout the U.S. Rural hospices, in particular, do not enjoy large patient censuses and are responsible for covering large geographic areas. Such a substantial new line item is not one such providers can comfortably cover.
Dr. Martha Twaddle, medical director of Barrington, Illinois-based JourneyCare, says she is concerned about what some hospices may do to survive. “In the past, we may have allowed a patient to continue on a medication rather than engage in a negotiation. Now, because of this financial pressure, some hospices will be forced to be more forthright in stopping medications not shown to be helpful,” Twaddle says.
Financial pressures, however, may impact the supply of medications that are actually needed. “They may try to substitute less expensive medications that are not as effective, and you don’t want to be monkeying around when someone is dying,” she says.
Administrative: The interest of Part D plans is not always best served by expediency. Theresa Forester, of the National Organization for Home Care and Hospice, says the opportunities for misunderstanding are numerous- and of concern to patients and families.
“There are incentives in the system that could lead Part D plans to drag their heels in terms of coverage, because in some instances, someone else might pick up the tab,” Forester says. “If there is a delay in payment, oftentimes family members will step up and pay out-of-pocket.” As patients and their families await resolutions in payer disputes, those families able to afford medication may feel urgency to cover drug costs themselves. Those unable to afford the coverage may face unnecessary stress or pressure to purchase medications and worry about the bill later– in some instances, arriving after a loved one’s death.
JourneyCare reports the average length of time for admissions visits has increased, and case managers and interdisciplinary teams must spend more time in homes sorting through medications and explaining to patients what medications may or may not be necessary. Penny Murphy, Vice President of Quality and Compliance, says much work is being done to proactively communicate with Part D plans. “I think the smaller programs have not had the resources to reach out and make those decisions,” Murphy says.
If patients are asked to stop medications they have been using for years – and aren’t receiving thorough explanations about the reasons why that drug for a thyroid condition may not be so important after a hospice enrollment – such administrative lack of capacity could cause undue stress or confusion. “Why do we need to add more stress when people are in a time of tough decisions?” Twaddle asks. “It’s just one more hoop to jump through.”
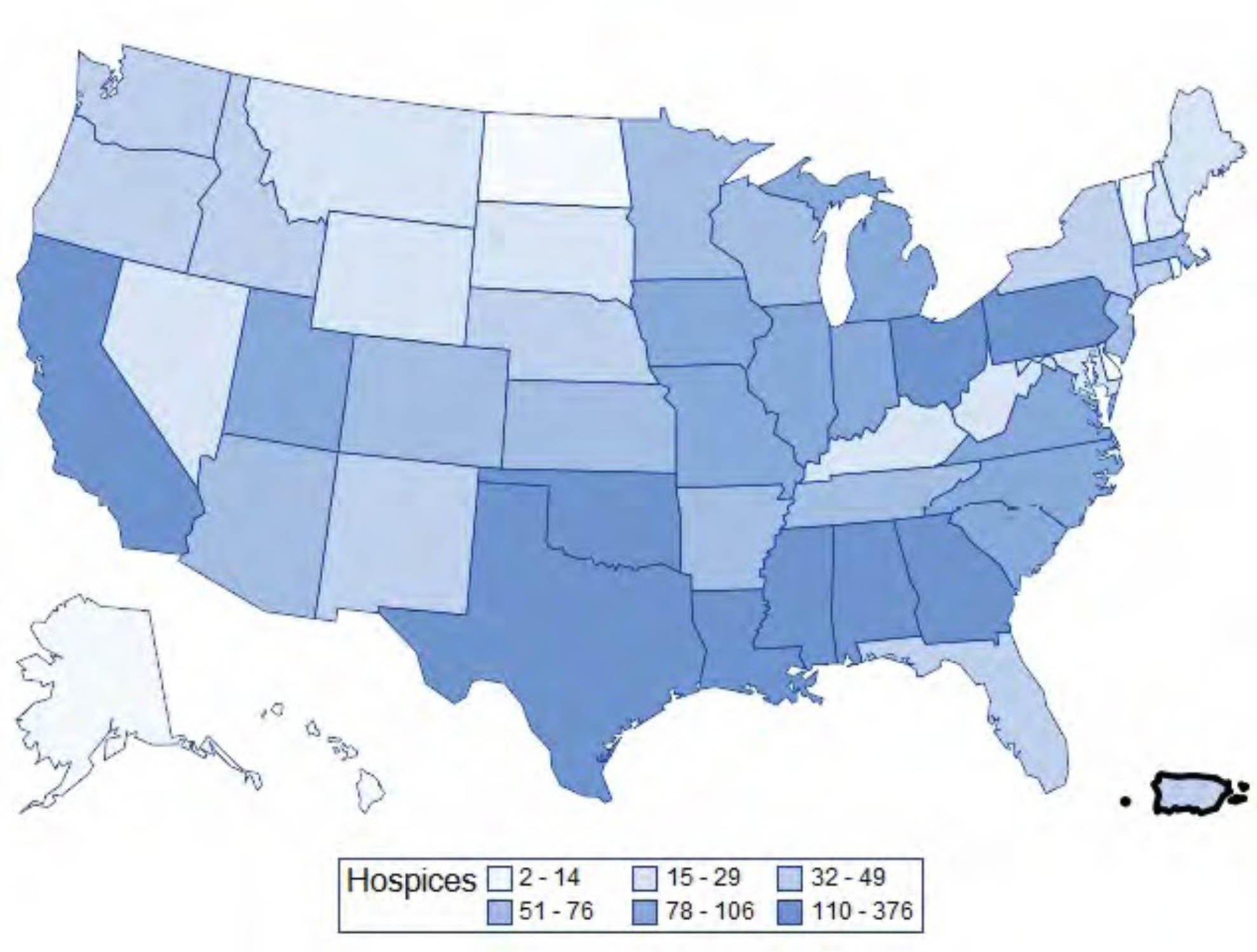
Access to Care: While some smaller hospices, such as Angels Grace, report decisions to cover all medications in these first weeks of the new rule, it is uncertain how long such a policy can be maintained. If pressures result in financial failure, hospices in aforementioned rural areas may be forced to close, cutting off vital resources for terminally ill patients with fewer care options. Hospices may also opt to turn down admissions from “complex patients” with multiple conditions the provider cannot afford to address. Both long-term implications are dire, reducing patient choice and access.
Should hospices be forced to enact more stringent reviews of medication regimens upon admission, Dr. Robert Arnold, of the University of Pittsburgh Center for Bioethics and Health Law, says this policy puts providers in the position of “being the bad guy.” This practice would further common – and incorrect – beliefs about hospice services. “The problem, particularly for smaller hospices, is their complex patients with medications that are expensive,” Arnold says. “The patients are scared about stopping them for symbolic value, which is psychologically difficult, or they feel better when they are on those medications.” Such sentiments could stand in the way of a choice to opt for hospice support.
Arnold says this CMS effort places problems within our larger health system on hospice providers. “It feels unfair, because they weren’t involved in starting these medicines.”

